Primary hydatid cyst of thigh: a rare case report
Agrawal S.1, Sharda P.2*, Gupta G.3, Gupta S.4, Kundal A.5
DOI: https://doi.org/10.17511/ijpr.2020.i01.07
1 Sonam Agrawal, Senior Resident, Department of Pediatrics, All India Institute of Medical Science, Rishikesh, Uttarakhand, India.
2* Prateek Sharda, Assistant Professor, Department of General Surgery, All India Institute of Medical Science, Rishikesh, Uttarakhand, India.
3 Gaurav Gupta, Department of General Surgery, All India Institute of Medical Science, Gorakhpur, Uttar Pradesh, India.
4 Sangeeta Gupta, Department of Physiology, All India Institute of Medical Science, Gorakhpur, Uttar Pradesh, India.
5 Ashikesh Kundal, Department of General Surgery, All India Institute of Medical Science, Gorakhpur, Uttar Pradesh, India.
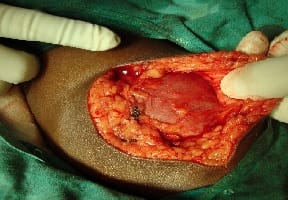
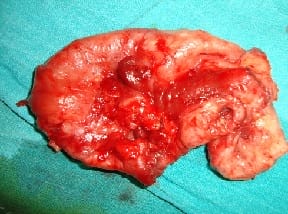
Primary hydatid cyst elsewhere in the body is rare, as these cysts are always secondary to a hydatid of the liver or lungs. We report a case of 14-year-old girl presented with a swelling on medial aspect of left upper thigh which was gradually increasing in size since last 12 months. Ultrasonography diagnosed it as hydatid cyst, there was no swelling in the liver, lungs or elsewhere in the body, CT scan further reinforced the diagnosis. The swelling was removed en bloc and albendazole was given.
Keywords: Primary Hydatid cyst, Daughter cyst, Albendazole, Echinococcus
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of General Surgery, All India Institute of Medical Science, Rishikesh, Uttarakhand, India. Email: |
Agrawal S, Sharda P, Gupta G, Gupta S, Kundal A. Primary hydatid cyst of thigh: a rare case report. Pediatric Rev Int J Pediatr Res. 2020;7(1):39-41. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/571 |


 ©
©