No pain, much to gain!!
Ranganath K. R.1, M. Prabhu S.2*, T. Kumar P.3, Govindaraj M.4
DOI: https://doi.org/10.17511/ijpr.2020.i07.01
1 Ranganath K. R., Associate Professor, Department of Paediatrics, Dr. B R Ambedkar Medical College, Bengaluru, Karnataka, India.
2* Sameeta M. Prabhu, Post-Graduate, Department of Paediatrics, Dr. B R Ambedkar Medical College, Bengaluru, Karnataka, India.
3 Pavan T. Kumar, Post-Graduate, Department of Paediatrics, Dr. B R Ambedkar Medical College, Bengaluru, Karnataka, India.
4 M. Govindaraj, Professor and HOD, Department of Paediatrics, Dr. B R Ambedkar Medical College, Bengaluru, Karnataka, India.
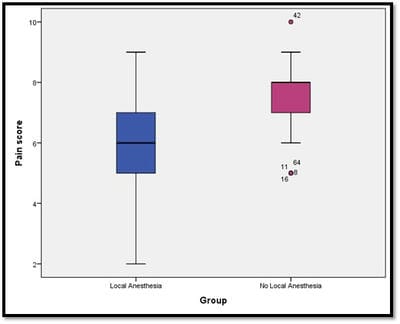
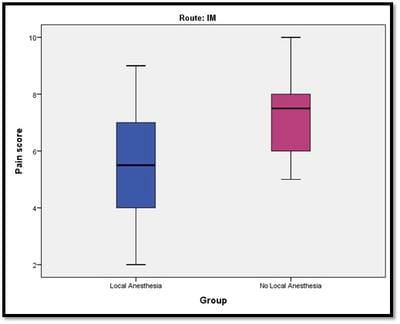
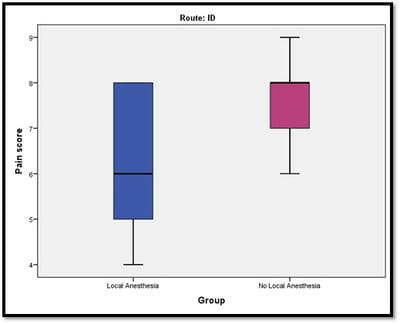
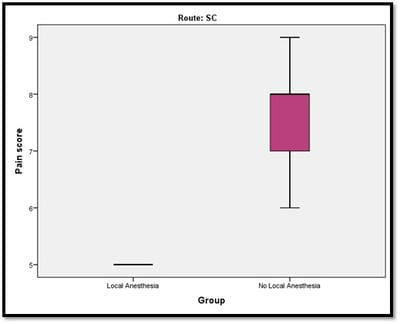
Background: Vaccination is an integral aspect of a pediatrician's practice. The fear associated with pain is a common problem. Alleviating this pain, not only puts the child at ease but also reduces the apprehension some parents have. Our objective was to evaluate local analgesic use during childhood immunization, its efficacy, and assessing how it serves as an advantage to the patient, the parents/guardian, and the medical personnel. Methodology: It was a randomized study. Data was collected for a period of 1 year, from August 2018 to August 2019. Children from birth to 18 years were divided into 2 groups: case (local anesthetic i.e Lidocaine aerosol applied) and control (no local anesthetics applied). They were immunized as per NIS/IAP. The pain was assessed by a standard pain chart (Modified Behavioural Pain Scale (BPS). Result: Totally (including IM, SC, and ID injections), the Local anesthesia group Median pain score was 6 and the No Local anesthesia group Median pain score was 8. There was a significant difference in pain scores between the two groups. Conclusion: The present study showed that local anesthetics could be applied quickly and with ease. There was a significant difference in pain scores between the two groups (higher score being in the group in which local anesthetics weren’t used). The reduction in the pain score, in turn, showed a significant difference in the attitude of the child, parent, as well as medical personnel.
Keywords: Vaccination, Pain, Local anesthetic
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Post-Graduate, Department of Paediatrics, Dr. B R Ambedkar Medical College, Bengaluru, Karnataka, India. Email: |
Ranganath KR, Prabhu SM, Kumar PT, Govindaraj M. No pain, much to gain!!. Pediatric Rev Int J Pediatr Res. 2020;7(7):317-325. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/600 |


 ©
©