Study of foot length measurement as a screening tool to identify low birth weight and preterm neonates
Mehta R.1, Dhaneria M.2, Prajapati J.3*
DOI: https://doi.org/10.17511/ijpr.2020.i07.04
1 Rishika Mehta, Senior Resident, Department of Paediatrics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
2 Mamta Dhaneria, Professor and Head, Department of Paediatrics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
3* Jyoti Prajapati, Assistant Professor, Department of Pediatrics, MGM Medical College and MY Hospital, Indore, Madhya Pradesh, India.
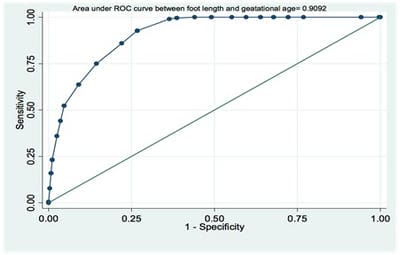
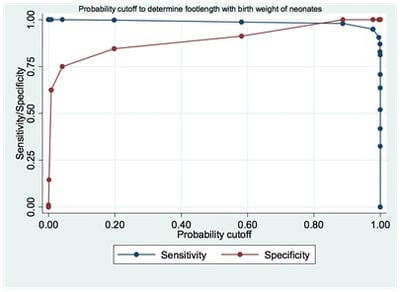
Introduction: Low birth weight is an important indicator of survival, future growth, and overall development of the child. It is associated with socio-economic, clinical, racial, hereditary, personal, and geographical factors. Method: This prospective observational study was conducted during the 19 months in the nursery and postnatal wards at RDGMC, Ujjain. All live birth newborns were assessed within 24 hours of birth. All Sick babies requiring NICU care, newborns with congenital malformation were excluded from the study. For each newborn recruited in the study length of the left foot was measured from the heel to the tip of the big toe using a hard transparent plastic ruler which was pressed vertically against the babies’ sole and the reading was recorded. The data was analyzed in Epidata (version 3.1) and then transferred to Stata10.0 (Stata Corp College Station, Texas, U.S.A) for statistical analysis. Results: (1) Foot length measurement was directly correlated with gestational age with cut off being 6.3 cm for 32 weeks,6.6 cm for 36 weeks, and 7.35 cm for > 36 weeks. (2) Foot length measurement directly correlated with the birth weight with the cut off for VLBW babies being 6.25 cm, for weight< 2000gm being 6.78 cm and LBW being 7.92 cm. Conclusion: Present study strongly recommends foot length measurement as an easy, fast, accurate, and low-cost tool for predicting prematurity and low birth weight not only in the hospital setup but also for community health providers.
Keywords: Preterm, foot length, screening tool, Low birth weight, preterm
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pediatrics, MGM Medical College and MY Hospital, Indore, Madhya Pradesh, India. Email: |
Mehta R, Dhaneria M, Prajapati J. Study of foot length measurement as a screening tool to identify low birth weight and preterm neonates. Pediatric Rev Int J Pediatr Res. 2020;7(7):337-343. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/622 |


 ©
©