Tracheal agenesis: a rare congenital disorder
Gundapuneni Rao R.1, Susarla Venkata Rama B.2*, Gattu H.3, Paripati A.4
DOI: https://doi.org/10.17511/ijpr.2021.i02.01
1 Ravali Gundapuneni Rao, Fellow in Neonatology, Department of Neonatal Intensive care unit, Ankura hospital for women and children, Hyderabad, Telangana, India.
2* Balaji Susarla Venkata Rama, Consultant Neonatologist, Department of Neonatal Intensive care unit, Ankura hospital for women and children, Hyderabad, Telangana, India.
3 Harshitha Gattu, Consultant Neonatologist, Department of Neonatal Intensive care unit, Ankura hospital for women and children, Hyderabad, Telangana, India.
4 Alekya Paripati, Junior Medical Officer, Department of Neonatal Intensive care unit, Ankura hospital for women and children, Hyderabad, Telangana, India.
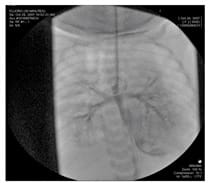
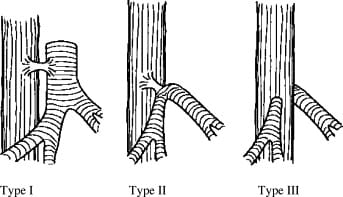
Tracheal agenesis is a severe congenital disorder with often an emergency presentation. There is a complete or partial absence of the trachea below the larynx, with the presence or absence of a tracheoesophageal fistula. It is a rare differential diagnosis of postnatal respiratory distress and the obstetrician or neonatologist will regularly be surprised by this malformation. The etiology of Tracheal atresia is unknown, therapeutic options are limited thus making this condition a usually fatal disorder. In most cases, congenital anomalies of the heart, digestive tract or GUT are present. The main signs are respiratory distress and cyanosis, inability to vocalize and impossible tracheal intubation. Isolated tracheal agenesis without any malformation is very rare. Here we report a case of a preterm neonate born at 33 weeks gestation with tracheal agenesis with no other associated malformation. In most cases, the seldom deformation, tracheal agenesis does not get recognized before the child is born.
Keywords: Tracheal agenesis, Congenital airway obstruction, Delivery room respiratory emergency
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Consultant Neonatologist, Department of Neonatal Intensive care unit, Ankura hospital for women and children, Hyderabad, Telangana, India. Email: |
Rao RG, Rama BSV, Gattu H, Paripati A. Tracheal agenesis: a rare congenital disorder. Pediatric Rev Int J Pediatr Res. 2021;8(2):68-71. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/663 |


 ©
©