Closure of a large upper muscular ventricular septal defect in a 2.3 kg baby using a duct occluder
Mohd Kamran M.1*, Abqari S.2, Haseen A.3, Yadav M.4
DOI: https://doi.org/10.17511/ijpr.2021.i03.07
1* Mirza Mohd Kamran, Assistant professor, Department of Pediatric Cardiology, PCE CS unit, JNMCH, AMU, Aligarh, Uttar Pradesh, India.
2 Shaad Abqari, Associate Professor, Department of Pediatrics, JNMCH, AMU, Aligarh, Uttar Pradesh, India.
3 Azam Haseen, Professor and Chairman, Department of CTVS, JNMCH, AMU, Aligarh, Uttar Pradesh, India.
4 Mayank Yadav, Assistant Professor, Department of CTVS, JNMCH, AMU, Aligarh, Uttar Pradesh, India.
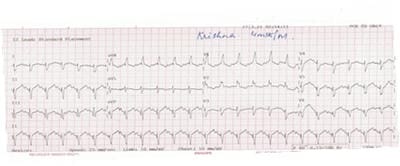
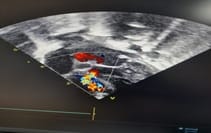
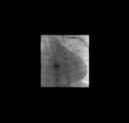
Surgical closure of the ventricular septal defect is a time tested and well-accepted procedure to date especially in smaller babies with failure to thrive and severe pulmonary hypertension. Surgical closure is regarded as the gold standard treatment. However over the past 10 years percutaneous trans-catheter device closure has emerged as a safer alternative especially in the case of muscular VSD. Transcatheter closure of ventricular septal defects (VSD) has not yet received general acceptance. It is not well-established in the younger age group with a weight category of less than 5kg. Occasionally, a hybrid procedure has been proposed. We believe that certain types of VSD can be closed safely by the transcatheter approach even if weight is less than 5kg, especially if the trend of miniaturizing devices continues. This approach should be considered as a valid alternative to a surgical option. We are reporting such a VSD baby with a weight of 2.3 Kg at the age of 6 months, which was closed with a duct occluder.
Keywords: Failure to thrive, Large VSD, Severe PAH, Transcatheter closure
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant professor, Department of Pediatric Cardiology, PCE CS unit, JNMCH, AMU, Aligarh, Uttar Pradesh, India. Email: |
Kamran M, Abqari S, Haseen A, Yadav M. Closure of a large upper muscular ventricular septal defect in a 2.3 kg baby using a duct occluder. Pediatric Rev Int J Pediatr Res. 2021;8(3):163-167. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/670 |


 ©
©