A Case of Anterior Mediastinal Mass treated as Bronchial Asthma.
Jadhav R.1, Motwani P.2*, Agarkhedkar S.3
DOI: https://doi.org/10.17511/ijpr.2021.i04.07
1 Renuka Jadhav, Professor, Department of Pediatrics, Dr D Y Patil Medical College, Pune, Maharastra, India.
2* Pooja Motwani, Resident, Department of pediatrics, Dr D Y Patil Medical College, Pune, Maharashtra, India.
3 Sharad Agarkhedkar, Head of the Department, Department of pediatrics, Dr D Y Patil Medical College, Pune, Maharashtra, India.
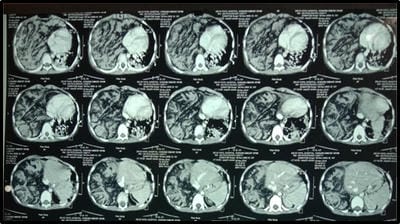
Anterior Mediastinal Masses (AMM) can range in presentation from an asymptomatic incidental finding to significant cardiorespiratory compromise. Symptoms do not always correlate to the degree of compression. Patients with AMM are at high risk for hemodynamic instability and cardiovascular arrest with induction of anesthesia. This report describes a child with a large AMM who presented with classic symptoms of recurrent wheezing and was inadequately evaluated. It is imperative, especially in these unexpected presentations, to have a high index of suspicion.
Keywords: Anterior Mediastinal Mass, Recurrent wheezing, Thymic Lymphoma
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of pediatrics, Dr D Y Patil Medical College, Pune, Maharashtra, India. Email: |
Renuka Jadhav, Pooja Motwani, Sharad Agarkhedkar, A Case of Anterior Mediastinal Mass treated as Bronchial Asthma.. Pediatric Rev Int J Pediatr Res. 2021;8(4):207-211. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/680 |


 ©
©