Ashy Dermatosis – A rare case in a 7year old Indian male child
Sandeep B.1, Shefali P.2*, Kiran B.3, Namitha.4
DOI: https://doi.org/10.17511/ijpr.2022.i05.03
1 B Sandeep, Professor, Department of Pediatrics, East Point College of Medical Sciences & RC, Bangalore, Karnataka, India.
2* P Shefali, Assistant Professor, Department of Pediatrics, East Point College of Medical Sciences & RC, Bangalore, Karnataka, India.
3 B Kiran, Professor & HOD, Department of Pediatrics, East Point College of Medical Sciences & RC, Bangalore, Karnataka, India.
4 Namitha, Assistant Professor, Department of Dermatology, East Point College of Medical Sciences & RC, Bangalore, Karnataka, India.
Ashy dermatosis also known as erythema dyschromicum perstans, is an acquired chronic pigmentary skin disorder. This disorder has been very rarely reported in Indian children. Here we report a case of a 7year old male child presented to pediatrics OPD with multiple areas of hyperpigmentation. A skin biopsy was done which was suggestive of Ashy dermatosis. Early recognition of this condition is important for proper diagnosis and to prevent unnecessary investigations.
Keywords: lichen planus pigmentosus, erythema dyschromicum perstans, ashy dermatosis, skin biopsy, hyperpigmentation
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pediatrics, East Point College of Medical Sciences & RC, Bangalore, Karnataka, India. Email: |
B Sandeep, P Shefali, B Kiran, Namitha, Ashy Dermatosis – A rare case in a 7year old Indian male child. Pediatric Rev Int J Pediatr Res. 2022;9(5):46-50. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/732 |


 ©
© 
 Figure 4: hyperpigmented mark with erythematous margin visible over the medial side of left knee joint
Figure 4: hyperpigmented mark with erythematous margin visible over the medial side of left knee joint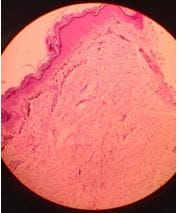 Figure 5: Histopathological examination of biopsy section of the erythematous lesion suggestive of hyperkeratosis of the epidermis with focal vacuolar degeneration of basal layer. The dermis shows increased pigment incontinence and mild perivascular infiltrate.
Figure 5: Histopathological examination of biopsy section of the erythematous lesion suggestive of hyperkeratosis of the epidermis with focal vacuolar degeneration of basal layer. The dermis shows increased pigment incontinence and mild perivascular infiltrate.