Retinopathy of Prematurity and Its Association with Oxygen Therapy in Preterm Low Birth Weight Babies
Abstract
Background: Retinopathy of prematurity (ROP) is a preventable cause of blindness in premature, low birth weight (LBW) infants, driven by abnormal retinal vascular development. Oxygen therapy, though life-saving, is a key modifiable risk factor when unmonitored, leading to retinal damage through disrupted angiogenesis. ROP follows a two-phase pathogenesis involving initial vessel growth suppression due to hyperoxia, followed by hypoxia-induced neovascularization. In countries like Bangladesh, rising preterm survival without adequate neonatal care infrastructure has increased ROP incidence.
Aim of the study: This study aims to investigate the association between oxygen therapy and the development of ROP in preterm, low-birth-weight infants.
Methods: This cross-sectional observational study was conducted in the NICU of (name) in Bangladesh to assess the prevalence of ROP and its association with oxygen therapy among 50 preterm, low-birth-weight infants. Eligible neonates (<37 weeks, <2500g, oxygen-exposed, and screened for ROP) were enrolled over a defined study period of (duration), from (start) to (end). Data were collected using structured forms covering clinical, demographic, and treatment details. ROP screening followed standard protocols using indirect ophthalmoscopy. Oxygen therapy mode and duration were recorded. Statistical analysis was performed using SPSS v26.0, applying descriptive statistics and chi-square/Fisher’s exact tests, with significance set at p < 0.05.
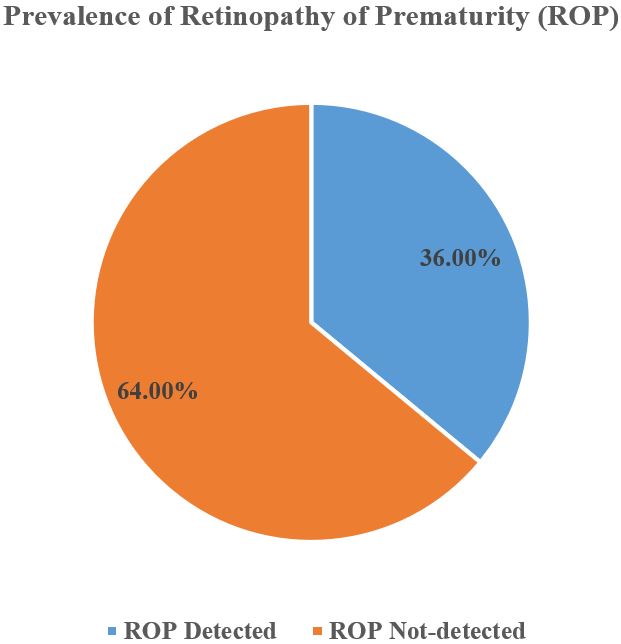
Results: Among 50 preterm low birth weight infants, 36% developed retinopathy of prematurity (ROP). Most were male (56%), born at 28–31 weeks (48%), and weighed 1000–1499 g (64%). CPAP was the most common oxygen modality (48%), with a mean oxygen duration of 5.8±2.3 days. ROP primarily involved Zone II (61.1%) and Stages 1–2. Bilateral ROP occurred in 61.1%, and 50% of cases required treatment. A significant association was found between oxygen therapy and ROP (p=0.04), especially with prolonged exposure (≥5 days; p=0.02) and mechanical ventilation (p=0.03), highlighting oxygen therapy as a key risk factor for ROP development.
Conclusion: This study highlights a significant association between unregulated oxygen therapy and ROP in preterm, low-birth-weight infants. Improved oxygen monitoring, adherence to saturation targets, and early ROP screening are essential to prevent vision loss. Strengthening neonatal care protocols can reduce the burden of this preventable cause of childhood blindness.
Downloads
References
2. Gilbert C. Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early human development. 2008 Feb 1;84(2):77-82.
3. Fierson WM, American Academy of Pediatrics Section on Ophthalmology, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, American Association of Certified Orthoptists, Chiang MF, Good W, Phelps D, Reynolds J, Robbins SL, Karr DJ. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2018 Dec 1;142(6):e20183061.
4. Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatric research. 2013 Dec;74(1):35-49.
5. Hartnett ME. Pathophysiology and mechanisms of severe retinopathy of prematurity. Ophthalmology. 2015 Jan 1;122(1):200-10.
6. Smith LE. Pathogenesis of retinopathy of prematurity. InSeminars in neonatology 2003 Dec 1 (Vol. 8, No. 6, pp. 469-473). WB Saunders.
7. Chow LC, Wright KW, Sola A, CSMC Oxygen Administration Study Group. Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants?. Pediatrics. 2003 Feb 1;111(2):339-45.
8. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: preliminary results. Pediatrics. 1988 May 1;81(5):697-706.
9. Hardy R, Good W, Dobson V, Palmer E, Tung B, Phelps D. Early Treatment for Retinopathy of Prematurity Cooperative GroupRevised indications for the treatment of retinopathy of prematurity. Results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121(12):1684-94.
10. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network. Target ranges of oxygen saturation in extremely preterm infants. New England Journal of Medicine. 2010 May 27;362(21):1959-69.
11. Ahmed AN, Muslima H, Anwar KS, Khan NZ, Chowdhury MA, Saha SK, Darmstadt GL. Retinopathy of prematurity in Bangladeshi neonates. Journal of tropical pediatrics. 2008 Oct 1;54(5):333-9.
12. Darlow BA, Hutchinson JL, Henderson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ, Australian and New Zealand Neonatal Network. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics. 2005 Apr 1;115(4):990-6.
13. Graham EQ. Retinopathy ofprematurity: an epidemic in the making. Chinese medical journal. 2010 Oct 20;123(20):2929-37.
14. Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B, Bauer N. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian journal of ophthalmology. 2014 Jan 1;62(1):41-9.
15. Quinn GE, Chan RP. Retinopathy of prematurity. InAlbert and Jakobiec's Principles and Practice of Ophthalmology 2022 Apr 23 (pp. 6737-6764). Cham: Springer International Publishing.
16. STOP-ROP Multicenter Study Group. Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics. 2000 Feb 1;105(2):295-310.
17. Tin W, Gupta S. Optimum oxygen therapy in preterm babies. Archives of Disease in Childhood-Fetal and Neonatal Edition. 2007 Mar 1;92(2):F143-7.
18. World Health Organization. WHO recommendations on interventions to improve preterm birth outcomes. InWHO recommendations on interventions to improve preterm birth outcomes 2015.
19. Dutta S, Narang S, Narang A, Dogra M, Gupta A. Risk factors of threshold retinopathy of prematurity. Indian pediatrics. 2004 Jul 1;41(7):665-72.
20. Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, Zin A, International NO-ROP Group. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005 May 1;115(5):e518-25.
21. Holmström G, El Azazi M, Jacobson L, Lennerstrand G. A population based, prospective study of the development of ROP in prematurely born children in the Stockholm area of Sweden. British journal of ophthalmology. 1993 Jul 1;77(7):417-23.
22. HA MH. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603-15.
23. Lee J, Chin JH, Kim JI, Lee EH, Choi IC. Association between red blood cell transfusion and long-term mortality in patients with cancer of the esophagus after esophagectomy. Diseases of the Esophagus. 2018 Feb 1;31(2):dox123.
24. Rivera JC, Holm M, Austeng D, Morken TS, Zhou T, Beaudry-Richard A, Sierra EM, Dammann O, Chemtob S. Retinopathy of prematurity: inflammation, choroidal degeneration, and novel promising therapeutic strategies. Journal of neuroinflammation. 2017 Dec;14:1-4.
Copyright (c) 2025 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


