Determinants of bottle feeding among 0- 24 months children
Kalpesh Makwana N.1*
DOI: https://doi.org/10.17511/ijpr.2020.i01.03
1* Namrata Kalpesh Makwana, Assistant Professor, Department of paediatrics, Shree M.P. Shah Medical College, Jamnagar, Gujarat, India.
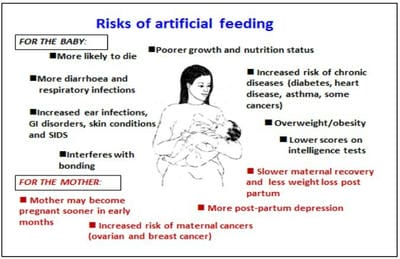
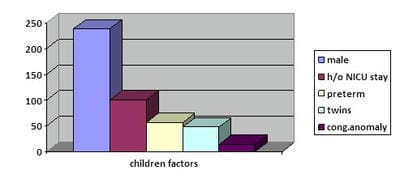
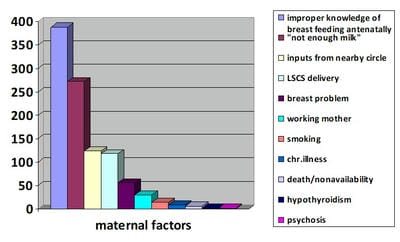
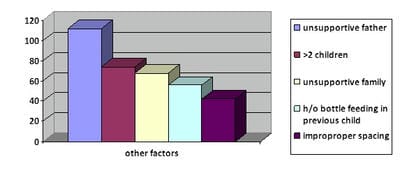
Background: To study various determinants of bottle feeding like factors related to children, mother and other factors. Methods: cross sectional study done from February 2019 to November 2019. A total 390 children were included in this study. Children who were 0-24 months & anytime bottle fed during this period and who were attending pediatric department of G.G. Govt. hospital & One private hospital, were enrolled. Data collected by interviewer & entered in case record sheet. Results: M:F ratio is 1.56. Bottle feeding seen in all socio-economic classes with highest rate in upper socio-economic class I. History of NICU stay was found in 25.6%. Percentage of preterm, twins & congenital anomaly are 14.4,12.3 & 3.6 respectively. Most mothers are 20-34 age & nonworking. About 30.3% had history of LSCS. About 14.4% have breast problem & 69.7% mothers had belief of “Not enough milk”. Maternal death/non availability, hypothyroidism, chronic illness, smoking & psychosis seen in only 1.5,0.5,2.1,3.6 & 0.5 percentage respectively. 99.5% mothers don’t have proper knowledge of breastfeeding in antenatal period. 31.8% mothers got inputs from nearby circle to start bottle feeding. 28.79% have unsupportive father & 17.48% have unsupportive family.19.02% have >2 kids. 10.8% does not have proper spacing. 14.4% shows previous h/o bottle feeding. Conclusions: Improper maternal knowledge regarding breast feeding, mothers’ belief of “Not enough milk”, inputs to start bottle from nearby circle, LSCS delivery, Male child, NICU stay, Unsupportive father & >2 kids are most eminent factors. There is a strong need for lactation guidance during antenatal period & breast-feeding counseling to mother, father and close family members.
Keywords: Bottle feeding, Determinants, Breastfeeding knowledge
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of paediatrics, Shree M.P. Shah Medical College, Jamnagar, Gujarat, India. Email: |
Makwana NK. Determinants of bottle feeding among 0- 24 months children. Pediatric Rev Int J Pediatr Res. 2020;7(1):14-21. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/553 |


 ©
©