Determinants of bottle feeding among 0-24 months children
Abstract
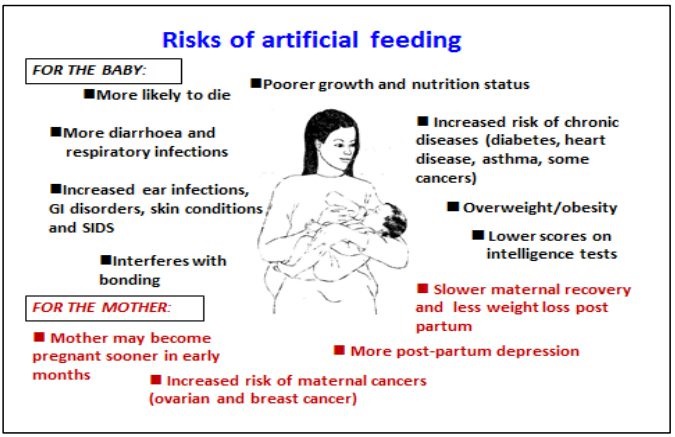
Background: To study various determinants of bottle feeding like factors related to children, mother and other factors.
Methods: cross sectional study done from February 2019 to November 2019. A total 390 children were included in this study. Children who were 0-24 months & anytime bottle fed during this period and who were attending pediatric department of G.G. Govt. hospital & One private hospital, were enrolled. Data collected by interviewer & entered in case record sheet.
Results: M:F ratio is 1.56. Bottle feeding seen in all socio-economic classes with highest rate in upper socio-economic class I. History of NICU stay was found in 25.6%. Percentage of preterm, twins & congenital anomaly are 14.4,12.3 & 3.6 respectively. Most mothers are 20-34 age & nonworking. About 30.3% had history of LSCS. About 14.4% have breast problem & 69.7% mothers had belief of “Not enough milk”. Maternal death/non availability, hypothyroidism, chronic illness, smoking & psychosis seen in only 1.5,0.5,2.1,3.6 & 0.5 percentage respectively. 99.5% mothers don’t have proper knowledge of breastfeeding in antenatal period. 31.8% mothers got inputs from nearby circle to start bottle feeding. 28.79% have unsupportive father & 17.48% have unsupportive family.19.02% have >2 kids. 10.8% does not have proper spacing. 14.4% shows previous h/o bottle feeding.
Conclusions: Improper maternal knowledge regarding breast feeding, mothers’ belief of “Not enough milk”, inputs to start bottle from nearby circle, LSCS delivery, Male child, NICU stay, Unsupportive father & >2 kids are most eminent factors. There is a strong need for lactation guidance during antenatal period & breast-feeding counseling to mother, father and close family members.
Downloads
References
National Family Health Survey – 4, 2015-16: India Fact Sheet, Ministry of Health and Family Welfare, Govt. Of India. Available from: http://rchips.org/NFHS/pdf/NFHS4/India.pdf. Accessed on Dec.17,2019.
Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: World Health Organisation; 2009.Session 2, The physiological basis of breastfeeding. Available at https://www.who.int/nutrition/publications/infantfeeding/9789241597494.pdf.
World Health Organisation (WHO) Maternal, Newborn, Child and Adolescent Health; Breastfeeding Geneva: WHO; 2016. Available at https://www.who.int/maternal_child_adolescent/en/.
Indian Academy of paediatrics (IAP) U.G. Teaching slide 2015-2016. Available at https://www.vims.ac.in/education/paediatrics-teaching-module.html.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, Rivera J. Maternal and child undernutrition: global and regional exposures and health consequences. The Lancet. 2008;371(9608):243-260. doi: https://doi.org/10.1016/s0140-6736(07)61693-6.
Victoria CG, Bahl R, Barros AJD, Franca GVA, Horton S, Krasevec J, Richter L. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475-490. doi: https://doi.org/10.1016/S0140-6736(15)01024-7.
World Health Organisation. WHO. Geneva, Switzerland, 2017. Guideline: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. Available at https://www.who.int/nutrition/publications/guidelines/breastfeeding-facilities-maternity-newborn/en/.
Lokare L, Hippargi A. Qualitative exploration of bottle-feeding practices among mothers of Dharwad district, Karnataka: a focus group discussion study, Int J Comm Med Public Heal. 2016;3(1):90-93. doi: https://doi.org/10.18203/2394-6040.ijcmph20151477.
Breastfeeding counselling: A training course. Geneva, WHO.1993. (WHO/CDR/93.6) Available at https://www.who.int/maternal_child_adolescent/documents/who_cdr_93_3/en/.
Chen CH, Wang TM, Chang HM, Chi CS. The effect of breast- and bottle-feeding on oxygen saturation and body temperature in preterm infants. J Hum Lact. 2000;16(1):21-27. doi: https://doi.org/10.1177/089033440001600105.
Carrascoza KC, Possobon Rde F, Tomita LM, Moraes AB. Consequences of bottle-feeding to the oral facial development of initially breastfed children. J Pediatr (Rio J). 2006;82(5):395-7. doi: https://doi.org/10.2223/JPED.1536. Epub 2006 Sep 21.
WHO. Infant and Young Child Feeding Indicators.2018. Available from: http://www.who.int/nutrition/databases/infantfeeding/key_databases/en/index1.html.
Pandey Vk, Aggrawal P, Kakkar R.Modified BG Prasad Socio-economic Classification, Update-2019. Indian J Comm Health.2019;31(1):123-125.
Gabriela dos Santos Buccini, Maria Helene D’Aquino Benicio, and Sonia Isoyama Venancio. Determinants of using pacifier and bottle feeding. Rev Saude Publica. 2014;48(4):571-582. doi: https://doi.org/10.1590/S0034-8910.2014048005128.
Hazir T, Akram DS, Nisar YB, Kazmi N, Agho KE, Abbasi S, et al. Determinants of suboptimal breast-feeding practices in Pakistan. Public Health Nutr. 2013;16(4):659-672. doi: http://dx.-doi.org/10.1017/S1368980012002935.
Mihrshahi S, Kabir I, Roy SK, et al. Determinants of infant and young child feeding practices in Bangladesh: secondary data analysis of Demographic and Health Survey 2004. Food Nutr Bull. 2010;31(2):295-313. doi: http://dx.-doi.org/10.1177/15642651003100220.
Berde AS. Factors Associated with Bottle Feeding in Namibia: Findings from Namibia 2013 Demographic and Health Survey. J Trop Pediatr. 2018;64(6):460-467. doi: https://doi.org/10.1093/tropej/fmx091.
Yokoyama Y, Ooki S. Breast-feeding and bottle-feeding of twins, triplets and higher order multiple births. Jap J Pub Health.2004;51(11):969-974.
Yokoyama Y, Wada S, Sugimoto M, Katayama M, Saito M, Sono J. Breastfeeding rates among singletons, twins and triplets in Japan: a population-based study. Twin Res Human Genet. 2005;9(2):298-302. doi: https://doi.org/10.1375/183242706776382347.
Sield SS, Muluneh E, Sinbirro IA, Moga TT, Haso TK, et al. Utilisation of bottle-feeding practices and associated factors among mothers who have infant less than 12 months of age in Agaro Town, Jimma Zone South West Ethiopia, 2018. Health Sci J 2019;13(1):630.
Boerma JT, Rutstein SO, Sommerfelt AE, Ibro SA. Bottle use for infant feeding in developing countries: data from the demographic and health surveys: had the bottle battle been lost? J Trop Pediatr. 1991;37(3):116-120. doi: https://doi.org/10.1093/tropej/37.3.116.
Hassan AA, Taha Z, Abdulla MA, Ali AA, Adam I. Assessment of Bottle-Feeding Practices in Kassala, Eastern Sudan: A Community-Based Study. Open Access Maced J Med Sci. 2019;7(4):651-656. doi: https://doi.org/10.3889/oamjms.2019.132.
Ipsa Mohapatra and Adrija Roy.Breastfeeding awareness and perception among antenatal mothers: A cross-sectional study in urban slum population of Bhubaneshwar, Odisha. J Edu Health Promot. 2018;7:60. doi: https://doi.org/10.4103/jehp.jehp_98_17.
Zhang K, Tang L, Wang H, Qiu L, Binns CW, Lee AH. Why do mothers of young infants choose to formula feed in china? perceptions of mothers and hospital staff. Int J Environ Res Public Health.2015;12 (5):4520-32. https://doi.org/10.3390/ijerph 120504520.
Kebebe T, Assaye H. Intention, magnitude and factors associated with bottle feeding among mothers of 0-23 months old children in Holeta town, Central Ethiopia: a cross sectional study. BMC Nutr. 2017;53. doi: https://doi.org/10.1186/s40795-017-0174-y.
Rahman A, Akter F. Reason for formula feeding among Bangladeshi mothers: A qualitative exploration. PLoS One. 2019;14(2):e0211761. doi: https://doi.org/10.1371/journal.pone.0211761.
Hackett KM, Mukta US, Jalal CSB, Sellen DW. A qualitative study exploring perceived barriers to infant feeding and care giving among adolescent girls and young woman in rural Bangladesh. BMC Public Health. 2015;15:771. doi: https://doi.org/10.1371/journal.pone.0211761.
Datta J, Graham B, Wellings K. The role of fathers in breastfeeding: Decision-making and support. Brit J Midwifery.2012;20(3):159-167. doi: https://doi.org/10.12968/bjom.2012.20.3.159
Victoria CG, Behague DP, Barros FC, Olinto MTA, Weiderpass E. Pacifier use and short breastfeeding duration: cause, consequence, or coincidence? Pediatr. 1997;99(3):445-453. doi: https://doi.org/10.1542/peds.99.3.445.
Araujo MFM, Schmitz BAS. Doze anos de evolucao da iniciativa Hospital Amigo da Crianca no Brasil. Rev Panam Salud Publica. 2007;22(2):91-99. doi: https://doi.org/10.1590/S1020-49892007000700003.
Vivienne A. Rose, Verlyn O.F. Warrington, Rolend Linder, Connie S. Williams. J Natl Med Assoc. 2004;96(3):325-331.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


