Clinico-pathological profile of paediatric patients with thalassemia major
Sharma S.1, Tikkas R.2*, Uikey R.3, Kumar V.4
DOI: https://doi.org/10.17511/ijpr.2020.i02.01
1 Shweta Sharma, Associate Professor, Department of Pediatrics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
2* R. Tikkas, Professor, Department of Pediatrics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
3 Rajni Uikey, Postgraduate, Department of Pediatrics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
4 Vinay Kumar, Postgraduate, Department of Pediatrics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
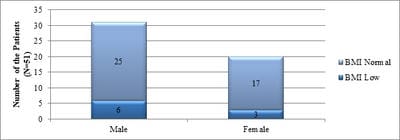
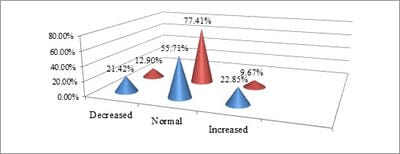
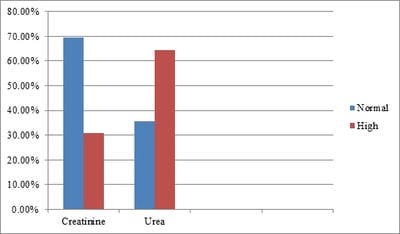
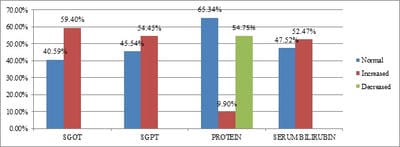
Background: The average prevalence of beta-thalassemia major is 3-4% which translates to 35-45 million carriers. Repeated use of blood transfusion in these patients causes significant morbidity and associated adverse effects. Aims and Objective: To study the clinical profile and laboratory parameters of Thalassemia major patients between the age group 1-14 years. Methodology: A Descriptive Observational study was done on 101 children of Beta-thalassemia major patients aged between 1-14 yr being regularly transfused at the Department of Pediatrics, Kamla Nehru Hospital, Gandhi Medical College, Bhopal, during the study period of March 2017 to Feb 2018. This included history, anthropometry, clinical examinations (general and systemic examinations) and laboratory Investigations including serum ferritin. RESULT: result showed that 42% patients were found to be underweight, 26.73% were short stature, 31.68% were hypocalcemic, 44.5% had low serum alkaline phosphatase. Transfusion frequency and serum ferritin were less in 1-5 years. A significant correlation was observed between the size of the spleen and the level of ferritin. CONCLUSION: Hereby it can be concluded that early diagnosis of the disease and early institution of chelation therapy can improve the life expectancy of the Beta-thalassemia patients.
Keywords: Beta-thalassemia, Ferritin, Splenomegaly, Chelation, Transfusion
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Pediatrics, Gandhi Medical College, Bhopal, Madhya Pradesh, India. Email: |
Sharma S, Tikkas R, Uikey R, Kumar V. Clinico-pathological profile of paediatric patients with thalassemia major. Pediatric Rev Int J Pediatr Res. 2020;7(2):49-55. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/573 |


 ©
©