Clinico-pathological profile of paediatric patients with thalassemia major
Abstract
Background: The average prevalence of beta-thalassemia major is 3-4% which translates to 35-45 million carriers. Repeated use of blood transfusion in these patients causes significant morbidity and associated adverse effects.
Aims and Objective: To study the clinical profile and laboratory parameters of Thalassemia major patients between the age group 1-14 years.
Methodology: A Descriptive Observational study was done on 101 children of Beta-thalassemia major patients aged between 1-14 yr being regularly transfused at the Department of Pediatrics, Kamla Nehru Hospital, Gandhi Medical College, Bhopal, during the study period of March 2017 to Feb 2018. This included history, anthropometry, clinical examinations (general and systemic examinations) and laboratory Investigations including serum ferritin.
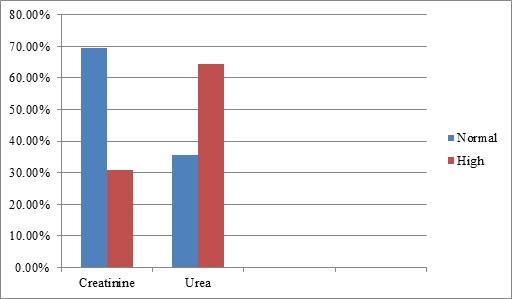
RESULT: result showed that 42% patients were found to be underweight, 26.73% were short stature, 31.68% were hypocalcemic, 44.5% had low serum alkaline phosphatase. Transfusion frequency and serum ferritin were less in 1-5 years. A significant correlation was observed between the size of the spleen and the level of ferritin.
CONCLUSION: Hereby it can be concluded that early diagnosis of the disease and early institution of chelation therapy can improve the life expectancy of the Beta-thalassemia patients.
Downloads
References
Thakur S, Sharma R, Sharada R. Incidence of Thalassemia and Sickle Cell Disease in Chhattisgarh, Central India: Using Hardy-Weinberg Equations. J Mol Gen Med.2014;9:155. doi: https://doi.org/10.4172/1747-0862.1000155.
Al-Salehe QAA, Al-Awady MS, Abbass SK. Growth Retardation In Β-Thalassemia Major: Iraqi PG Med J. 2015;14(2).
Shah N, Mishra A, Chauhan D, Vora C, Shah NR. Study on effectiveness of transfusion program in thalassemia major patients receiving multiple blood transfusions at a transfusion centre in Western India. Asian J Transfus Sci. 2010;4(2):94-98. Available from: http://www.ajts.org/text.asp?2010/4/2/94/67029.
Hassan MY, Max J Coppes: emedicine, Medscape; Aug 23, 2017. Available from https://emedicine.medscape.com/article/958850-clinical.
Ali S, Jahan S. Growth Failure in β-Thalassemia major Patients Undergoing Repeated Transfusions. JIIMC. 2016;11(3):120-124.
El-Nashar M, Mortagy AK, El-Beblawy NM, El-Gohary E, Kamel IM, Rashad M, et al. Parathyroid hormone in pediatric patients with β-thalassemia major and its relation to bone mineral density; a case control study. Egypt J Med Human Genet. 2017;18(1):75-78. doi: http://dx.doi.org/10.1016/j.ejmhg.2016.03.004.
Goyal M, Abrol P, Lal H. Parathyroid and Calcium Status in Patients with Thalassemia. Indian J Clin Biochem. 2010;25(4):385-387. doi: https://dx.doi.org/10.1007%2Fs12291-010-0071-5.
Vogiatzi MG, Autio KA, Mait JE, Schneider R, Lesser M, Giardina PJ. Low bone mineral density in adolescents with β‐thalassemia. Annals New York Acad Sci. 2005;1054(1):462-466. doi: https://doi.org/10.1196/annals.1345.063.
Soliman A, Sanctis VD, Yassin M. Vitamin D Status in Thalassemia Major: an Update. Mediterr J Hematol Infect Dis. 2013;5(1):e2013057. doi: https://dx.doi.org/10.4084%2FMJHID.2013.057.
Teli AB, Deori R, Saikia SP, Pathak K, Panyang R, Rajkakati R. β-Thalassaemia and its Co-existence with Haemoglobin E and Haemoglobin S in Upper Assam Region of North Eastern India: A Hospital Based Study. J Clin Diagn Res. 2016;10(4):GC01-GC04. doi: https://doi.org/10.7860/JCDR/2016/16265.7675.
Sultan S, Irfan SM, Ahmed SI. Biochemical Markers of Bone Turnover in Patients with β-Thalassemia Major: A Single Center Study from Southern Pakistan. Advan Hematol. 2016. doi: https://doi.org/10.1155/2016/5437609.
Smolkin V, Halevy R, Levin C, Mines M, Sakran W, Ilia K, et al. Renal function in children with beta-thalassemia major and thalassemia intermedia. Pediatr Nephrol. 2008;23(10):1847-1851. doi: https://doi.org/10.1007/s00467-008-0897-8.
Jalali A, Khalilian H, Ahmadzadeh A, Sarvestani S, Rahim F, Zandian K, et al. Renal function in transfusion dependent pediatric beta-thalassemia major patients. Hematol. 2011;16(4):249-254. doi: https://doi.org/10.1179/102453311X12953015767662.
Hamed EA, ElMelegy NT. Renal functions in pediatric patients with beta-thalassemia major: relation to chelation therapy: original prospective study. Italian J Pediatr. 2010;36:39. doi: https://doi.org/10.1186/1824-7288-36-39.
Quinn CT, Johnson VL, Kim HY, Trachtenberg F, Vogiatzi MG, Kwiatkowski JL, et al. Renal dysfunction in patients with thalassaemia. Br J Haematol. 2011;153(1):111-117. doi: https://dx.doi.org/10.1111%2Fj.1365-2141.2010.08477.x.
Lai ME, Spiga A, Vacquer S, Carta MP, Corrias C, Ponticelli C. Renal function in patients with β-thalassaemia major: a long-term follow-up study. Nephrol Dial Transplant. 2012;27(9):3547-3551. doi: https://doi.org/10.1093/ndt/gfs169.
Mishra AK, Tiwari A. Iron Overload In Beta Thalassaemia Major And Intermedia Patients. Maedica: J Clinic Med. 2013;8(4):328-332.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


