Transfusion practices in the pediatric and neonatology departments of Soavinandriana hospital center
Lalao Tsifiregna R.1*, Rakotomahefa Narison M.2, Nambininjanahary F.3, Lalaina Robinson A.4, Rakoto Alison O.5
DOI: https://doi.org/10.17511/ijpr.2020.i05.04
1* Rosa Lalao Tsifiregna, Department of Pediatrics and Neonatology, Hospital Center of Soavinandriana, Antananarivo, Madagascar. 2 Mbola Rakotomahefa Narison, Pediatric Oncology Pilot Unit, Joseph Ravoahangy Andrianavalona Hospital Center, Antananarivo, Madagascar. 3 Filaminantsoa Nambininjanahary, Department of Pediatrics and Neonatology, Hospital Center of Soavinandriana, Antananarivo, Madagascar. 4 Annick Lalaina Robinson, Child Mother Hospital, Anatananarivo, Madagascar. 5 Olivat Rakoto Alison, Hematology Unit, Joseph Ravoahangy Andrianavalona Hospital Center, Antananarivo, Madagascar.
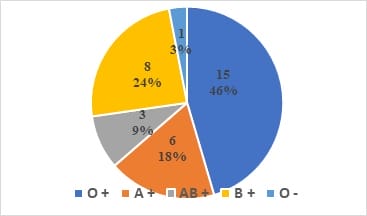
Blood transfusion is an important part of day-to-day clinical practice. The main objective of this work is to describe transfusion practices in the Pediatrics and Neonatology Department of the Hospital Center of Soavinandriana. Methods: A prospective observational study of 6 months has been conducted. All requests to Department of Pediatrics and Neonatology for blood for transfusion for children aged less than 14 years were identified prospectively. The variables studied were: patients’ characteristics (age, gender) reason for hospitalization, paraclinical examinations (blood count and formula before transfusion, ABO and Rhesus grouping), the presented pathology, the indicated transfusion: nature, incidents during and after transfusion and the outcome of the pathology (healing, death). Results: The incidence was 6.54%, 33 patients had a blood transfusion. The sex ratio was 1.35. The average age is 46.06 months. Skin pallor was the main reason for hospitalization, which represented 18.18% of the cases. The average hemoglobin level was 8.08 g/dl. The O and rhesus positive blood group was the predominant in this work. The blood products which were used were: red blood cell (n=20, 54.05%), whole blood (n=15, 40.54%), fresh frozen plasma (n=1, 2.70%), platelets concentrate (n=1, 2.70%). Conclusion: The packed red blood cell was used the most and the hospital blood bank did not have enough labile blood products. It is therefore essential to improve the structures for the preparation of blood and its derivatives, in order to make all varieties of labile blood products accessible.
Keywords: Blood transfusion, Practices, Antananarivo
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of Pediatrics and Neonatology, Hospital Center of Soavinandriana, Antananarivo, Madagascar. Email: |
Tsifiregna AL, Narison MR, Nambininjanahary F, Robinson AL, Alison OR. Transfusion practices in the pediatric and neonatology departments of Soavinandriana hospital center. Pediatric Rev Int J Pediatr Res. 2020;7(5):210-216. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/582 |


 ©
©