To study the clinical profile and early outcome of term asphyxiated newborns intramurally and extramurally in SNCU, Dr. Bram Hospital, Raipur, Chhattisgarh, India
Rathi Y.1*
DOI: https://doi.org/10.17511/ijpr.2020.i04.03
1* Yogita Rathi, Resident, Department of Paediatrics, Pt J.N.M. Medical College, Raipur, Chhattisgarh, India.
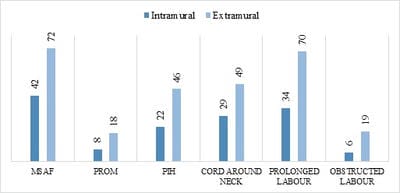
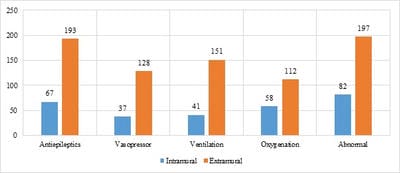
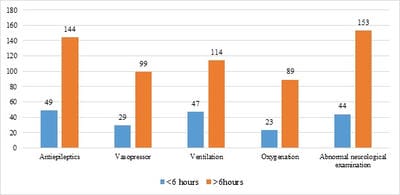
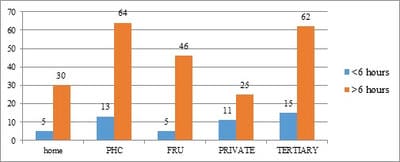
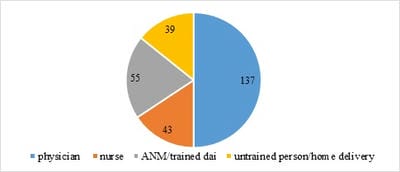
Introduction: Perinatal asphyxia is an important contributor of neonatal morbidity, mortality and adverse outcome in India. Aim and Objective: To study the clinical profile and early outcome of term asphyxiated newborns intramurally and extramurally. Material and Methods: Cross-sectional observational hospital-based study was conducted over a period of one year from January 2018 to December 2018 in Special Newborn Care Unit (SNCU) of Dr BRAM Hospital, Raipur, Chhattisgarh. Sarnat and Sarnat staging was used to classify HIE. Statistical analysis was performed by using SPSS21.0 software. Chi-square test, P-value and likelihood ratio were calculated using appropriate tests. Result: Total 2035 newborns were admitted in SNCU during the study period. 415 newborns were admitted with HIE.66.03% newborns were extramural and 33.97% were intramural.71% of extramural babies admitted to neonatal ward after 6 hours. This is showing delayed or inaccurate identification of the gravity of the situation, inaccurate diagnosis and in many cases delayed referral and transport to an appropriate referral centre. 242(58.3%) were HIE II followed by 121(29.1%) were HIE-III and rest 52 (12.5%) were HIE-I cases.the mortality rate in extramural babies was 35.67% and intramural babies were 13.47%. Conclusion: The study has shown the significant differences that account in the antenatal and perinatal profile, perinatal management and resuscitation, postnatal management, morbidity, mortality and neurodevelopment outcome of extramurally delivered neonates in comparison to institutional deliveries.
Keywords: Meconium stained liquor (MSAF), Hypoxic Ischemic Encephalopathy (HIE), Special Newborn Care Unit (SNCU)
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of Paediatrics, Pt J.N.M. Medical College, Raipur, Chhattisgarh, India. Email: |
Rathi Y. To study the clinical profile and early outcome of term asphyxiated newborns intramurally and extramurally in SNCU, Dr. Bram Hospital, Raipur, Chhattisgarh, India. Pediatric Rev Int J Pediatr Res. 2020;7(4):174-180. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/588 |


 ©
©