To study the clinical profile and early outcome of term asphyxiated newborns intramurally and extramurally in SNCU, Dr. Bram Hospital, Raipur, Chhattisgarh, India
Abstract
Introduction: Perinatal asphyxia is an important contributor of neonatal morbidity, mortality and adverse outcome in India.
Aim and Objective: To study the clinical profile and early outcome of term asphyxiated newborns intramurally and extramurally.
Material and Methods: Cross-sectional observational hospital-based study was conducted over a period of one year from January 2018 to December 2018 in Special Newborn Care Unit (SNCU) of Dr BRAM Hospital, Raipur, Chhattisgarh. Sarnat and Sarnat staging was used to classify HIE. Statistical analysis was performed by using SPSS21.0 software. Chi-square test, P-value and likelihood ratio were calculated using appropriate tests.
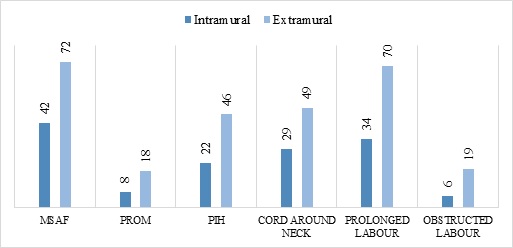
Result: Total 2035 newborns were admitted in SNCU during the study period. 415 newborns were admitted with HIE.66.03% newborns were extramural and 33.97% were intramural.71% of extramural babies admitted to neonatal ward after 6 hours. This is showing delayed or inaccurate identification of the gravity of the situation, inaccurate diagnosis and in many cases delayed referral and transport to an appropriate referral centre. 242(58.3%) were HIE II followed by 121(29.1%) were HIE-III and rest 52 (12.5%) were HIE-I cases.the mortality rate in extramural babies was 35.67% and intramural babies were 13.47%.
Conclusion: The study has shown the significant differences that account in the antenatal and perinatal profile, perinatal management and resuscitation, postnatal management, morbidity, mortality and neurodevelopment outcome of extramurally delivered neonates in comparison to institutional deliveries.
Downloads
References
Neonatal Morbidity and Mortality. Report of the National Neonatal Perinatal Database. Indian Pediatr.1999;36:167-169.
Reducing one million child deaths from birth asphyxia services of the health system, gaps an priorities: Health Research Policy System.2007;5:4. doi: https://dx.doi.org/10.1186%2F1478-4505-5-4.
Hoque M, Haaq S, Islam R. Causes of neonatal admissionsand deaths at a rural hospital in KwaZulu-Natal,South Africa. South African J Epidemiol Infect. 2011;26(1):26-29.https://doi.org/10.1080/10158782.2011.11441416.
Chishty AL, Iqbal MA, Anjum A, Maqbool S. Risk factor analysis of Birth Asphyxia at the Children`s Hospital, Lahore. Pak Paediatr J. 2002;26(2):47-53.
World Health Organization. Basic Newborn resus¬citation. A practical guide. World Health Organization; Geneva, 1997.Available athttps://www.who.int/maternal_child_adolescent/documents/who_rht_msm_981/en/.
Gupta BD, Sharma P, Bagla J, Parakh M, Soni JP. Renal failure in asphyxiated neonates. Indian Pediatr. 2005;42(9):928-934.
Martin-Ancel A, Garcia-Alix A, Gaya F, Cabañas F, Burgueros M. Multiple organ involvement in perinatal asphyxia. J Pediatr. 1995;127(5):786-793. doi: https://doi.org/10.1016/s0022-3476(95)70174-5.
Cohn HE, Sacks EJ, Heymann MA, Rudolph AM. Cardiovascular responses to hypoxemia and acidemia in fetal lambs. Am J Obstet Gynecol. 1974;120(6):817-824.doi: https://doi.org/10.1016/0002-9378(74)90587-0.
Rudolph AM. The fetal circulation and its response to stress. J Dev Physiol. 1984;6(1):11-19.
AzraHaider B, Bhutta ZA. Birth asphyxia in developing countries:Current status and public health implications. CurrProblPediatricsAdolesc Health Care. 2006;36(5):178‑188.doi: https://doi.org/10.1016/j.cppeds.2005.11.002.
Rana MN, Kazi MY, Nasir A. Outcome of babies admitted with hypoxic ischemic encephalopathy in neonatal unit of services Hospital, Lahore. Ann King Edward Med Coll. 2006;12(2):243-244. doi: https://doi.org/10.21649/akemu.v12i2.889.
Yelamali BC, Panigatti P, Pol R, Talawar KB, Naik S, Badakali A. Outcome of newborn with birth asphyxia in tertiary care hospital - a retrospective study. MedicaInnovatica. 2014;3(2):59-64.
Shrestha M, Shrestha L, Shrestha PS. Profile of asphyxiated babies at Tribhuvan university teaching hospital. J Nepal PaediatrSoc. 2009;29(1):3-5. doi: https://doi.org/10.3126/jnps.v29i1.1592.
Memon S, Shaikh S, Bibi S. To compare the outcome (early) of neonates with birth asphyxia in‐relation to place of delivery and age at time of admission J Pak Med Assoc. 2012;62(12):1277-1281.
Shireen N, Nahar N, Mollah AH. Risk factors and short-term outcome of birth asphyxiated babies in Dhaka medical college hospital. Bangladesh J Child Health. 2009;33(3):83-89.doi:https://doi.org/10.3329/bjch.v33i3.5688.
Mohan K, Mishra PC, Singh DK. Clinical profile of birth asphyxia in newborn. IntJ Sci Technol. 2013;3(1):10-19.
Sehgal A, Roy MS, Dubey NK, Jyothi MC. Factors contributing to outcome in neonates delivered out of hospital and referred to a teaching institution. Indian Pediatr. 2001;38(11):1289-1294.
Siva S SB, Nair CC, Madhu GN, Srinivasa S, Manjunath MN. Clinical profile and outcome of perinatal asphyxia in a tertiary care centre. CurrPediatr Res. 2015;19(1 & 2):9-12.
Majeed R, Memona Y, Majeed F. Risk factors for birth asphyxia. J Ayub Med Coll. Abbottabad. 2007;19(3):67-71.
Shah GS, Singh R, Das BK. Outcome of neonates with birth asphyxia. J Nepal Med Assoc. 2005;44(158):44-46.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


