Nutritional status characteristics of infants presenting with neonatal cholestasis
Kant Bharti L.1, Kishun J.2*
DOI: https://doi.org/10.17511/ijpr.2020.i05.02
1 Laxmi Kant Bharti, Additional Professor, Department of Pediatric Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences(SGPGI), Lucknow, Uttar Pradesh, India.
2* Jai Kishun, Assistant Professor, Department of Biostatistics and Health Informatics, Sanjay Gandhi Postgraduate Institute of Medical Sciences(SGPGI), Lucknow, Uttar Pradesh, India.
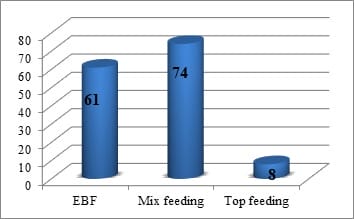
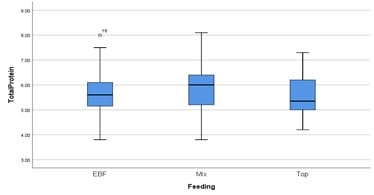
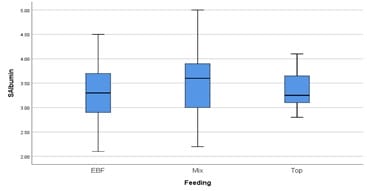
Background: Neonatal cholestasis (NC) is one of the commonest presentations in early infancy diseases. The nutritional status of infants may be affected by many factors. Impaired bile flow may further lead to the nutritional compromise of infants. Timely nutritional assessment and adequate nutritional support in the form of adequate breastfeeding and if required appropriate formulae feeding according to age and weight is crucial for better outcomes in improving morbidity and decreasing mortality of infants with NC. Methods: Consecutive 143 patients of NC up to 12 months enrolled from the HIS data (hospital information system). Anthropometric examination, mode, and type of feeding and serum markers like LFT (liver function test) and Hb (hemoglobin) were recorded. Data were analyzed by IAP growth parameters and SPSS 21. Results: The mean age of NC presentation was 3.6 months. 74(51.7%) were on mixed feeding, 61(42.6%) were exclusively breastfed (EBF) and only 8(5.6%) infants were on only top feeding by formula feeding or bovine milk feed. 39.16% were undernourished and around 19.5% were stunted.40% infants were anemic. The median value of serum albumin in top-fed and EBF (exclusive breastfed) was low. Conclusions: Malnutrition is common in infants with NC. There area different feeding pattern and type observed in infants with NC. EHBA (extrahepatic biliary atresia) is the most common diagnosis in infants with NC presented to the tertiary care center. Early nutritional assessment and timely nutritional supplementation having a crucial role in the outcome of patients with various diagnoses in NC.
Keywords: Neonatal cholestasis, Undernutrition, Breastfeeding, Nutritional status, Infant
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Biostatistics and Health Informatics, Sanjay Gandhi Postgraduate Institute of Medical Sciences(SGPGI), Lucknow, Uttar Pradesh, India. Email: |
Bharti LK, Kishun J. Nutritional status characteristics of infants presenting with neonatal cholestasis. Pediatric Rev Int J Pediatr Res. 2020;7(5):199-203. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/599 |


 ©
©