A pattern of poisoning in children- an experience from a teaching hospital in southern India
Vijayalakshmi P1, V. Benakanal S.2*, B. Patil R.3, Manoj GM4, S. Kumar R.5
DOI: https://doi.org/10.17511/ijpr.2020.i06.09
1 Vijayalakshmi P, Assistant Professor, Department of Paediatrics, SHIMOGA Institute of Medical Sciences, Shivamogga, Karnataka, India.
2* Shreeshail V. Benakanal, Assistant Professor, Department of Paediatrics, SHIMOGA Institute of Medical Sciences, Shivamogga, Karnataka, India.
3 Ravindra B. Patil, Professor and HOD, Department of Paediatrics, SHIMOGA Institute of Medical Sciences, Shivamogga, Karnataka, India.
4 Manoj GM, Senior resident, Department of Paediatrics, SHIMOGA Institute of Medical Sciences, Shivamogga, Karnataka, India.
5 R. Vikram S. Kumar, Professor, Department of Pediatrics, Subbaih Institute of Medical Sciences, Shivamogga, Karnataka, India.
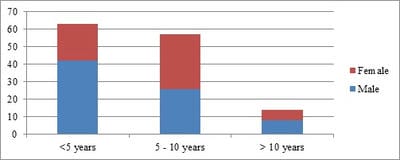
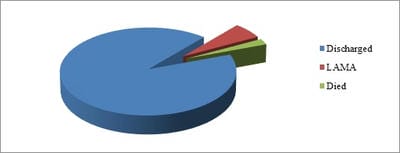
Introduction: Poisoning in children is an important Paediatric emergency and is a worldwide problem. It is a common and preventable cause of morbidity and mortality in children. Objectives: The aim of this study was to determine the profile and outcome of children less than 13 years admitted to the Paediatric department presenting with acute poisoning at a Teaching district hospital in southern Karnataka. Methods: Prospectively, 134 acute poisoning cases, admitted to Paediatric intensive care, SIMS Shivamogga from November 2018 to May 2019 were included in this study. Results: During the study period, 134 patients presented with acute poisoning. The incidence of poisoning in Paediatric patients was 2.84%. The median age of our patients was 5.2 years (range 0.75-12 years). The male to female ratio was 1.58:1. Animal bites (27.61%), Petroleum products (26.87%), Household chemicals (15.67%), Drugs (11.19%), Poisonous plant derivatives (8.96%) and Insecticides (6.72%) were the agents most frequently implicated. Almost all (98.41%) cases in 1 to 5 years age group were accidental in nature, whereas in the >10 years age group, the majority (71.43%) were suicidal. Thirteen patients (9.7%) remained asymptomatic. The specific antidote was given to 19 (14.18%) patients. Three patients (2 snake bite and 1 rodenticide child) died. The mean duration of hospital stay was 4.49 days (range was 1 day to 22 days). Conclusions: Accidental poisoning was common in children below 5 years of age. Minimal age of suicidal poisoning was 8 years. The most common agent implicated was a snake bite.
Keywords: Acute poisoning, Profile, Snakebite, Kerosene, Turpentine
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Paediatrics, SHIMOGA Institute of Medical Sciences, Shivamogga, Karnataka, India. Email: |
Vijayalakshmi P, Shreeshail V B, Ravindra B P, Manoj GM, Vikram RKS. A pattern of poisoning in children- an experience from a teaching hospital in southern India. Pediatric Rev Int J Pediatr Res. 2020;7(6):279-286. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/615 |


 ©
©