Compresetsive myelopathy presenting with paraparesis in pediatric age
Kotrashetti V. A.1, Baburao S V.2, Bainade K.3, Ravindran N S.4*, Vatkar A.5, Gupta S.6
DOI: https://doi.org/10.17511/ijpr.2020.i06.14
1 Kotrashetti V. A., Professor, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India.
2 Vijay Baburao Sonawane, Associate professor, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India.
3 Kapil Bainade, Assistant Professor, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India.
4* Shweta Ravindran Nair, Senior Resident, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India.
5 Amit Vatkar, Assistant Professor, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India.
6 Samarth Gupta, Junior resident, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India.
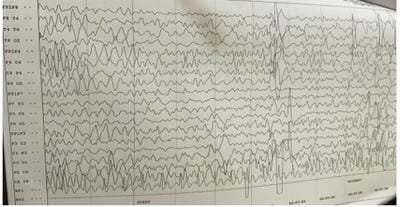
Compressive myelopathy is a common presentation of the adult age group secondary to degenerating etiologies. Trauma is a rare cause of compressive myelopathy, especially in the pediatric age group as the pediatric spine is more elastic than that of adults, especially below 8 years of age. Boys are more commonly injured as compared to girls. The present study reports a case of a six-year-old female patient of compressive myelopathy presenting with jerks with progressive paraparesis. MRI shows posterior subluxation of dens (C2) attached to C2 vertebral effacing anterior – subarachnoid space and indenting spinal cord.
Keywords: Spine injury, Dens dislocation, Atlanto-dental interval, Atlanto-axial fusion
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Pediatrics, DY Patil Hospital, Nerul, Maharashtra, India. Email: |
Kotrashetti V A, Sonawane VB, Bainade K, Nair S R, Vatkar A, Gupta S. Compresetsive myelopathy presenting with paraparesis in pediatric age. Pediatric Rev Int J Pediatr Res. 2020;7(6):313-316. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/616 |


 ©
©