Clinico-epidemiological profile of congenital heart disease in a tertiary care center – a retrospective descriptive study
Ramawat P.1, Jain N.2*
DOI: https://doi.org/10.17511/ijpr.2020.i07.02
1 Pramila Ramawat, Assistant Professor, Department of Pediatrics, MGM Medical College, Indore, Madhya Pradesh, India.
2* Nilesh Jain, Associate Professor, Department of Pediatrics, MGM Medical College, Indore, Madhya Pradesh, India.
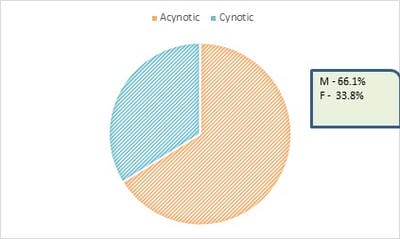
Aims and objective: To study the clinical-epidemiological profile of congenital heart disease in hospitalized children. Material and methods: A retrospective study was planned in a tertiary care center in Central India. Children between ages 1 month to 14 years with CHD were included in this study. Type of CHD, clinical presentation, anthropometry, demographic profile, and the outcome was recorded. Result: A total of 65 patients were included in the study. 43 patients were suffering from acyanotic CHD and 22 were having cyanotic CHD. Most of the children admitted were below 1 year of age (n-67%). Males (42) were more reported in the present study than females (23). Conclusion: CHDs are one of the commonest birth defects, timely diagnosis and intervention are very important to decrease mortality and morbidity in pediatric patients.
Keywords: CHD, Birth defect, Epidemiological
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Pediatrics, MGM Medical College, Indore, Madhya Pradesh, India. Email: |
Ramawat P, Jain N. Clinico-epidemiological profile of congenital heart disease in a tertiary care center – a retrospective descriptive study. Pediatric Rev Int J Pediatr Res. 2020;7(7):326-330. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/620 |


 ©
©