Mid-upper arm circumference cut-off for detection of severe acute malnutrition in infants aged between one and six months
S.D. J.1, L. Bendre S.2*, S. Desai A.3
DOI: https://doi.org/10.17511/ijpr.2020.i08.07
1 Jyothi S.D., Associate Professor, Department of Paediatrics, Belagavi Institute of Medical Sciences, Belagavi, Karnataka, India.
2* Spoorthi L. Bendre, Senior Resident, Department of Paediatrics, Mysore Medical College and Research Institute, Mysore, Karnataka, India.
3 Arunkumar S. Desai, Former Head of the Department, Department of Paediatrics, Belagavi Institute of Medical Sciences, Belagavi, Karnataka, India.
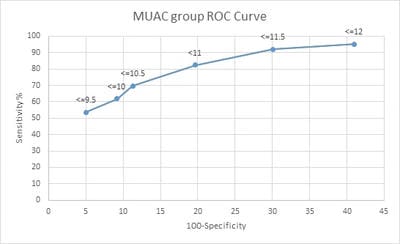
Objective: To find the MUAC cut-off for detection of severe acute malnutrition in infants between 1 to 6 months of age. Material and Methods: A prospective observational study at IPD and OPD of a tertiary care hospital. 303 infants between one and six months of age above the length of 45cms were included in the study. In infants between one and six months of age, the length, weight, and MUAC were measured. SAM infants were identified using the WHO definition. Sensitivity, specificity, and Youden index for a particular MUAC was calculated in SAM infants. Results: 11cms was found to have a sensitivity of 85.1% and specificity of 65.9%. It had the maximum Youden index of 0.55 with a positive likelihood ratio of 2.79 and a negative likelihood ratio of 0.21. Conclusions: MUAC of 11cms can be used as a cut-off for SAM infants between 1 to 6 months of age. MUAC does not vary with gender. Weight and MUAC are significantly lower in SAM infants. But there is no difference when it comes to length as in acute malnutrition, the weight and MUAC are affected but length is not.
Keywords: MUAC, Cut-off, SAM, Infants, Malnutrition, Severe acute malnutrition
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Paediatrics, Mysore Medical College and Research Institute, Mysore, Karnataka, India. Email: |
Jyothi SD, Bendre SL, Desai AS. Mid-upper arm circumference cut-off for detection of severe acute malnutrition in infants aged between one and six months. Pediatric Rev Int J Pediatr Res. 2020;7(8):430-436. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/643 |


 ©
©