Mid-upper arm circumference cut-off for detection of severe acute malnutrition in infants aged between one and six months
Abstract
Objective: To find the MUAC cut-off for detection of severe acute malnutrition in infants between 1 to 6 months of age.
Material and Methods: A prospective observational study at IPD and OPD of a tertiary care hospital. 303 infants between one and six months of age above the length of 45cms were included in the study. In infants between one and six months of age, the length, weight, and MUAC were measured. SAM infants were identified using the WHO definition. Sensitivity, specificity, and Youden index for a particular MUAC was calculated in SAM infants.
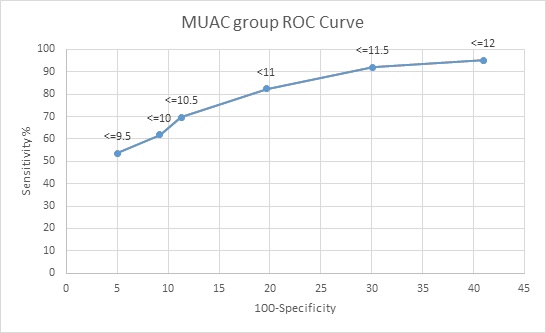
Results: 11cms was found to have a sensitivity of 85.1% and specificity of 65.9%. It had the maximum Youden index of 0.55 with a positive likelihood ratio of 2.79 and a negative likelihood ratio of 0.21.
Conclusions: MUAC of 11cms can be used as a cut-off for SAM infants between 1 to 6 months of age. MUAC does not vary with gender. Weight and MUAC are significantly lower in SAM infants. But there is no difference when it comes to length as in acute malnutrition, the weight and MUAC are affected but length is not.
Downloads
References
UNICEF, WHO, The World Bank; Levels and Trends in Child Malnutrition: UNICEF-WHO-World Bank Joint Child Malnutrition Estimates. 2017 May. Available at https://www.who.int/nutgrowthdb/jme_brochoure2017.pdf?ua=1.
NFHS 3 data, based on WHO 2006 growth standards compiled by WHO. Available at http://rchiips.org/nfhs/nfhs3.shtml.
NFHS 4 data, based on WHO 2006 growth standards compiled by WHO. Available at http://rchiips.org/nfhs/nfhs-4Reports/India.pdf.
Management of Acute Malnutrition in Infants (MAMI) project. Emergency Nutrition Network, UCL Centre for International Health and Development, Action Contre la Faim, 2010. Available at https://reliefweb.int/sites/reliefweb.int/files/resources/8A7E77D26B35660F492576F70010D7DF-mami-report-complete.pdf.
Lopirore C, Dop MC, Solal-Celigny A, Lagnado G. Excluding infants under 6 months of age from surveys: impact on prevalence of pre-school undernutrition. Public Health Nutr 2007;10(1):79-87. doi: 10.1017/S1368980007219676.
Vygen SB, Roberfroid D, Captier V, Kolsteren P. Treatment of severe acute malnutrition in infants aged <6 months in Niger. J Pediatr. 2013;162(3):515-521.e3. doi: 10.1016/j.jpeds.2012.09.008.
Berkley JA, Ngari M, Thitiri J, Mwalekwa L, Timbwa M, Hamid F. et al. Daily co-trimoxazole prophylaxis to prevent mortality in children with complicated severe acute malnutrition: a multicentre, double-blind, randomised placebo-controlled trial. Lancet Glob Health. 2016;4(7):e464-e473. doi: 10.1016/S2214-109X(16)30096-1.
Kerac M, Blencowe H, Grijalva-Eternid C, McGrath M, Shoham J, Cole TJ et al. Prevalence of wasting among under 6 month old infants in developing countries and implications of new case definitions using WHO growth standards: a secondary data analysis. Arc Dis Child. 2011;96(11):1008-1013. doi: 10.1136/adc.2010.191882.
Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006;27(3):S7-23. doi: 10.1177/15648265060273S302.
WHO. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva, World Health Organization; 2013. Available at https://www.who.int/publications/i/item/9789241506328.
Angood C, McGrath M, Mehta S, Mwangome M, Lung’ahoM, Roberfroid D et al. Research priorities to improve the management of acute malnutrition in infants aged less than six months (MAMI). PLoS Med.
;12(4):e1001812. doi: 10.1371/journal.pmed.1001812.
Blackwell N, Myatt M, Allafort-Duverger T, Balogoun A, Ibrahim A, Briend A. Mothers Understand And Can do it (MUAC): a comparison of mothers and community health workers determining mid-upper arm circumference in 103 children aged 6 months to 5 years. Arch Public Health. 2015;73(1):26. doi: 10.1186/s13690-015-0074-z.
Mwangome M, Ngari M, Fegan G, Mturi N, Shebe M, Bauni E, et al. Diagnostic criteria for severe acute malnutrition among infants aged under 6 mo. Am J Clin Nutr. 2017;105(6):1415-1423. doi: 10.3945/ajcn.116.149815.
Chand S, Shah D. Mid-upper arm circumference for detection of severe acute malnutrition in infants aged between one and six months. Indian Pediatr. 2015;52:528-529.
WHO. Facility based care of severe acute malnutrition. Country Office for India; 2013, March. Available at https://www.nhm.gov.in/images/pdf/programmes/child-health/IEC-materials/PARTICIPANT-MANUAL_FBCSA-Malnutrition.pdf.
WHO. WHO Child growth Standards. Available at https://www.who.int/tools/child-growth-standards.
Murphy M, Abebe K, Mahony S, Barthorp H, Andert C. Management of acute malnutrition in infants less than six months in a South Sudanese refugee population in Ethiopia. Field Exchange, 2017.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


