Mild cases of Covid-19 in children. is it really true or a mirage?
Mandal A.1*, Kondekar S.2, Bothara R.3
DOI: https://doi.org/10.17511/ijpr.2020.i08.10
1* Abhishek Mandal, Final MBBS year, TNMC and Nair Hospital, Mumbai, Maharashtra, India.
2 Santosh Kondekar, Associate professor, TNMC and Nair Hospital, Mumbai, Maharashtra, India.
3 Rishi Bothara, Final MBBS year, TNMC and Nair Hospital, Mumbai, Maharashtra, India.
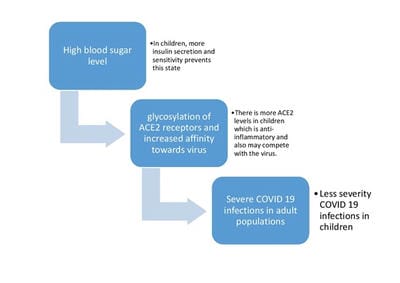
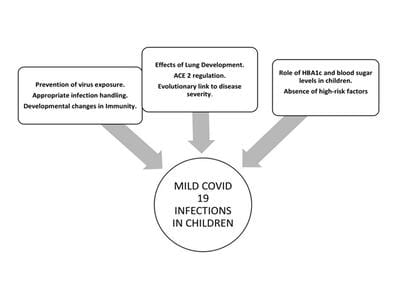
To date, very few data on pediatric COVID 19 cases have been published, and most reports originate from China. There is an urgent need to understand why the course of the coronavirus that started in late 2019 is affecting different groups of individuals with varying severity during the ongoing global pandemic. Globally, the greatest burden of most infectious diseases, especially infections of the respiratory system are borne by children, hence the low burden of COVID 19 in children has been viewed by many as surprising. This article will provide insights regarding the role of constitutional higher trained immunity in children, physiological advantages of children, higher insulin secretion, higher ACE2 levels, better antioxidant potential, and absence of high-risk factors in protecting children against severe COVID 19 infections.
Keywords: SARS-CoV2, Children, ACE2, Trained immunity, Antioxidant
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Final MBBS year, TNMC and Nair Hospital, Mumbai, Maharashtra, India. Email: |
Mandal A, Kondekar S, Bothara R. Mild cases of Covid-19 in children. is it really true or a mirage?. Pediatric Rev Int J Pediatr Res. 2020;7(8):446-451. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/644 |


 ©
©