A Pilot Study of the effects of Yoga Prana Vidya (YPV) protocols on social behaviour, cognitive abilities and IQ of mentally challenged children
Khatri R.1, Bembalkar S.2, Nanduri V.3*
DOI: https://doi.org/10.17511/ijpr.2021.i01.02
1 Rajkumari Khatri, Senior ENT & Head Neck Oncologist, YPV Trainer & Healer, Indore, Madhya Pradesh, India.
2 Shilpa Bembalkar, Technical officer(B), ICMR National AIDS Research Institute, Pune, Maharastra, India.
3* V S Nanduri, Consultant - Research & Publications, Yoga Prana Vidya ashram, Sri Ramana Trust, Thally, Tamilnadu, India.
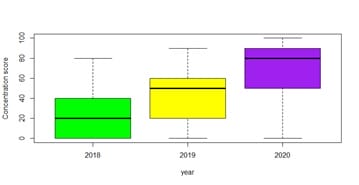
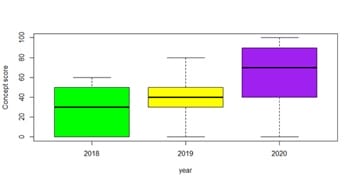
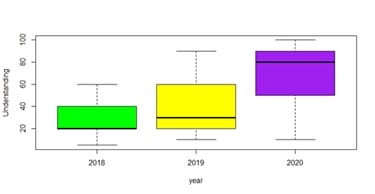
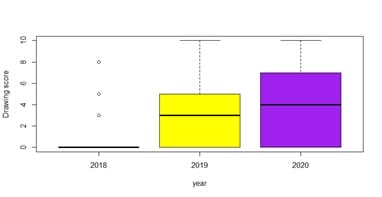
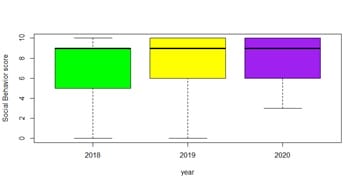
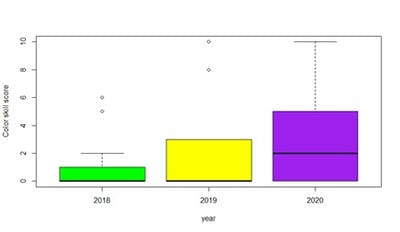
Introduction: Mental retardation is a neurodevelopmental disability of children. In this pilot study the authors have applied Yoga Prana Vidya system protocols for a pilot sample of mentally retarded children to study the effects and improvements in their being. Objectives: To assess (1) improvements of social behaviour, cognitive abilities and IQ, (2) reduction in morbidity, and (3) the effects on the frequency and duration of epilepsy attacks and seizures. Design: This is a longitudinal study of 2 years duration mixed methods design using YPV intervention on a selected pilot-scale sample, collecting data on qualitative observations of social behaviour, and measurements of cognitive abilities and IQ pre and post-test for quantitative analysis. Results: Statistical analysis of quantitative data revealed a significant increase in concentration, concept test, memory test, understanding, and social behavior. some increase in IQ and drawing test was present, however not found statistically significant. There was a reduction in the frequency and duration of epileptic attacks in epileptic children. Conclusion: This study has demonstrated that the YPV modality of complementary therapy has great utility and scope in improving the social behaviour, cognitive abilities and IQ of mentally challenged children. It is recommended that the earlier the intervention is conducted for the challenged children the better and sooner will be the better quality of life for them in terms of improved mental, emotional, and physical health. Further research with longitudinal fullscale studies is recommended to investigate this phenomenon widely.
Keywords: Mentally retarded children, epilepsy, yoga, meditation, Energy Healing, Complementary and Alternative Therapy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Consultant - Research & Publications, Yoga Prana Vidya ashram, Sri Ramana Trust, Thally, Tamilnadu, India. Email: |
Khatri R, Bembalkar S, Nanduri VS. Running Head: A pilot study on Yoga Prana Vidya for improvements in mentally Challenged children. Pediatric Rev Int J Pediatr Res. 2021;8(1):07-15. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/653 |


 ©
©