Assessment & correlation of gestational age in newborns with head circumference: A Hospital-based cross-sectional study in Central India
Shekhar Lohia P.1, Shrivastava V.2*, Sahu A.3
DOI: https://doi.org/10.17511/ijpr.2021.i02.07
1 Purnendu Shekhar Lohia, Assistant Professor, Department of Paediatrics, People’s College of Medical Sciences and Research Centre, Bhopal, Madhya Pradesh, India.
2* Vishal Shrivastava, Assistant Professor, Department of Paediatrics, People’s College of Medical Sciences and Research Centre, Bhopal, Madhya Pradesh, India.
3 Anita Sahu, Lecturer of Statistics, People’s College of Medical Sciences and Research Centre, Bhopal, Madhya Pradesh, India.
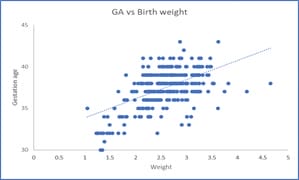
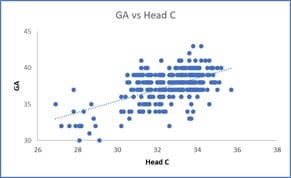
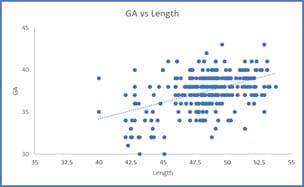
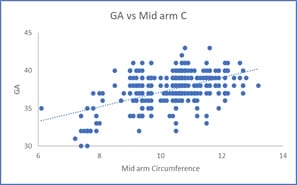
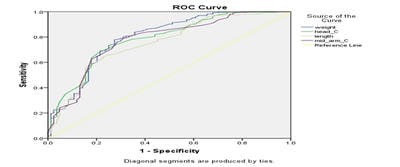
Introduction: Preterm birth is the leading cause of death in children younger than 5 years worldwide. Although preterm survival rates have increased in high-income countries, preterm newborns still die because of a lack of adequate newborn care in many low-income and middle-income countries. This study was aimed to find out the effectiveness of anthropometric measurement, a simple and inexpensive method, for identifying premature babies at birth. Method: We conducted a cross-sectional study in a tertiary care hospital with 350 consecutively live-born newborns. Their birth weight, mid-arm circumference, length and head circumference were measured and compared with gestational age assessed by New Ballard score. We summarized the variables using descriptive statistics, and the strength of association was determined through correlation analysis. The correlation was strong for head circumference. Linear regression analysis was done to develop predictive equations. Result: Amongst 350 newborns, 76% were term and 24% were preterm. Pearson's correlation coefficient between gestational age as assessed by New Ballard score and head circumference, birth weight, mid-arm circumference and length all showed a significant positive correlation in the decreasing order [maximum with head circumference (r = 0.566)]. Linear regression analysis was done to develop predictive equations. Conclusion: Head circumference measurement can be a surrogate marker to predict prematurity as a significant correlation is seen between it and gestational age assessed by the New Ballard score. Further studies are needed to cross-validate our result.
Keywords: Gestational age, Neonatal anthropometry, Prematurity
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Paediatrics, People’s College of Medical Sciences and Research Centre, Bhopal, Madhya Pradesh, India. Email: |
Lohia PS, Shrivastava V, Sahu A. Assessment & correlation of gestational age in newborns with head circumference: A Hospital-based cross-sectional study in Central India. Pediatric Rev Int J Pediatr Res. 2021;8(2):109-115. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/674 |


 ©
©