Chronic Subdural Hygroma in Battered Baby.
Bhaisare K.1*, Holikar S.2
DOI: https://doi.org/10.17511/ijpr.2021.i04.05
1* Kiran Bhaisare, Associate Professor, Department of Paediatrics, Vilasrao Deshmukh Institute of Medical science, Latur, Maharashtra, India.
2 Sunil Holikar, Associate Professor, Department of Paediatrics, Vilasrao Deshmukh Institute of Medical science, Latur, Maharashtra, India.
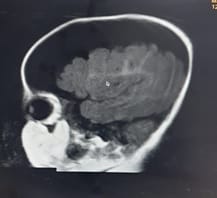
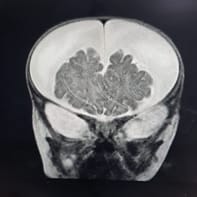
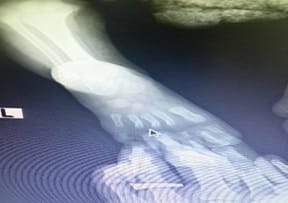
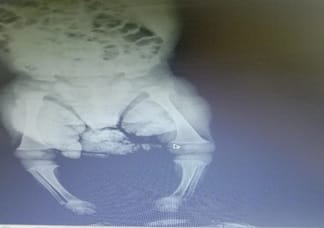
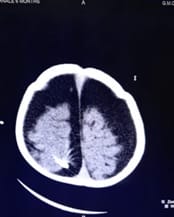
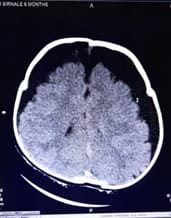
The battered baby syndrome is a condition in which a child is seriously physically abused by the caregiver or parents. The World Health Organization (WHO) estimates 40 million children are subjected to abuse and neglect around the world. Most of the industrialized countries have their reporting and surveillance system and data on child battery but in developing countries including India, there is a lack of data regarding the extent of child battering that takes place within the households or institutions. India published a report on one of the largest surveys done on child abuse and found that two out of every three children were physically abused and 88.6% of them suffered at the hands of their parents. Unfortunately, the methodology restricted the study to only older children who could give a history of abuse. Therefore, the magnitude of the problem given only highlights among children above the age of 5 years. [1]. we are reporting a case of an Infant with Febrile encephalopathy, detailed examination and investigation found out a case of chronic Subdural Hygroma with classical neuroimaging features of Abusive trauma. We have done a multidisciplinary approach with a Neurosurgeon, a social worker who treated the child with burr hole surgery for subdural hygroma & the child recovered with consciousness. This case is Special because a 5-month Male infant was subjected to abuse due to a psychological problem in a Family Member, suspicion was lacking as males are unlikely to undergo gender-biased in India and Early age of presentation.
Keywords: Abusive Head trauma, Febrile encephalopathy, Child Abuse, Multiple Fractures
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Paediatrics, Vilasrao Deshmukh Institute of Medical science, Latur, Maharashtra, India. Email: |
Kiran Bhaisare, Sunil Holikar, Chronic Subdural Hygroma in Battered Baby.. Pediatric Rev Int J Pediatr Res. 2021;8(4):196-200. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/690 |


 ©
©