Clinical, Microbiological and Radiological Characterises of Lower Respiratory tract Infection in Children with Established Congenital Heart Diseases.
Bhaskar S.1, Afzal K M.2*, Babu R M.3, Subramanya NK.4
DOI: https://doi.org/10.17511/ijpr.2021.i04.03
1 Sandeep Bhaskar, Associate professor, Department of Pediatrics, Vydehi Institute Of medical sciences, Bangalore, Karnataka, India.
2* Afzal K M, Senior Resident, Department of Pediatrics, Vydehi Institute of Medical Sciences, Bangalore, Karnataka, India.
3 Manjunatha Babu R, Professor, Department of Pediatrics, Akash Institute of medical sciences, Devanahalli, Karnataka, India.
4 Subramanya NK, Professor, Department of Pediatrics, Vydehi Institute Of medical sciences, Bangalore, Karnataka, India.
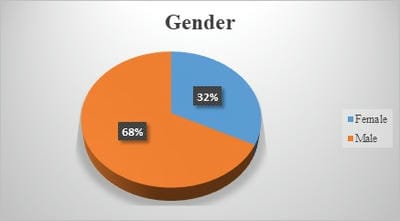
Introduction: Acute Lower Respiratory Tract Infection (ALRTI) is the most common cause of death in children under five. Various demographic, socio-economic and environmental factors have been associated with ALRTI, with conflicting results. Children with congenital heart diseases are more vulnerable to lower respiratory tract infections following the fact that they had an anatomical defect that causes hemodynamic disturbance of lung circulation and mucosal oedema finally leads to decreased lung compliance and recurrent lower respiratory tract infections. Methods: Children aged between1 month and 18 years with clinically established congenital heart disease confirmed by echocardiography and presenting with signs and symptoms suggestive of lower respiratory tract infection were enrolled in the study. A detailed history was taken and routine blood investigations were done in all cases. Chest X-Ray was done to confirm the clinical diagnosis. Results: Mean age of the study subjects was 2 years. VSD was seen in 64.9% of cases while 10.5% of cases had VSD and ASD. The most common presenting symptoms were: cough (98.2%), reduced feeding (97.4%), fever (89.5%), running nose (67.5%) and wheeze (49.1%). Leucocytosis and raised ESR were seen in 66.7% and 64.9% cases respectively. In Throat swab Commensals were seen in 36% of cases while gram-positive cocci were seen in 3.5% cases respectively. In blood culture Streptococcus pneumoniae being the commonest organism isolated. Bilateral and unilateral opacities on chest x-ray were seen in 16.7% and 12.3% cases respectively. Conclusion: Bronchopneumonia was the commonest LRTI in children with the predominance of VSD.
Keywords: LRTI, Congenital heart disease, Chest X-ray
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Pediatrics, Vydehi Institute of Medical Sciences, Bangalore, Karnataka, India. Email: |
Bhaskar S, Afzal K M, Babu RM, Subramanya NK. Clinical, Microbiological and Radiological Characterises of Lower Respiratory tract Infection in Children with Established Congenital Heart Diseases.. Pediatric Rev Int J Pediatr Res. 2021;8(4):182-188. Available From https://pediatrics.medresearch.in/index.php/ijpr/article/view/693 |


 ©
©