Clinical, Microbiological and Radiological Characterises of Lower Respiratory tract Infection in Children with Established Congenital Heart Diseases.
Abstract
Introduction: Acute Lower Respiratory Tract Infection (ALRTI) is the most common cause of death in children under five. Various demographic, socio-economic and environmental factors have been associated with ALRTI, with conflicting results. Children with congenital heart diseases are more vulnerable to lower respiratory tract infections following the fact that they had an anatomical defect that causes hemodynamic disturbance of lung circulation and mucosal oedema finally leads to decreased lung compliance and recurrent lower respiratory tract infections.
Methods: Children aged between1 month and 18 years with clinically established congenital heart disease confirmed by echocardiography and presenting with signs and symptoms suggestive of lower respiratory tract infection were enrolled in the study. A detailed history was taken and routine blood investigations were done in all cases. Chest X-Ray was done to confirm the clinical diagnosis.
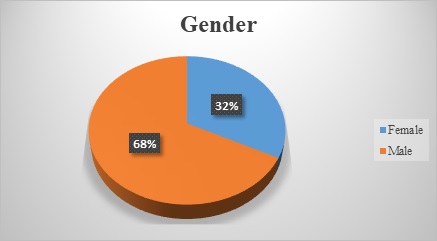
Results: Mean age of the study subjects was 2 years. VSD was seen in 64.9% of cases while 10.5% of cases had VSD and ASD. The most common presenting symptoms were: cough (98.2%), reduced feeding (97.4%), fever (89.5%), running nose (67.5%) and wheeze (49.1%). Leucocytosis and raised ESR were seen in 66.7% and 64.9% cases respectively. In Throat swab Commensals were seen in 36% of cases while gram-positive cocci were seen in 3.5% cases respectively. In blood culture Streptococcus pneumoniae being the commonest organism isolated. Bilateral and unilateral opacities on chest x-ray were seen in 16.7% and 12.3% cases respectively.
Conclusion: Bronchopneumonia was the commonest LRTI in children with the predominance of VSD.
Downloads
References
Broor S, Pandey RM, Ghosh M, Maitreyi RS, Lodha R, Singhal T, et al. Risk factors for severe acute lower respiratory tract infection in under-five children. Indian Pediatr. 2001 Dec;38(12):1361-9.
Graham NM. The epidemiology of acute respiratory infections in children and adults: a global perspective. Epidemiol Rev. 1990;12:149-78. doi: 10.1093/oxfordjournals.epirev.a036050.
Berman S. Epidemiology of acute respiratory infections in children of developing countries. Rev Infect Dis. 1991 May-Jun;13 Suppl 6:S454-62. doi: 10.1093/clinids/13.supplement_6.s454.
Cashat-Cruz M, Morales-Aguirre JJ, Mendoza-Azpiri M. Respiratory tract infections in children in developing countries. Semin Pediatr Infect Dis. 2005 Apr;16(2):84-92. doi: 10.1053/j.spid.2005.12.005.
Koch A, Mølbak K, Homøe P, Sørensen P, Hjuler T, Olesen ME, et al. Risk factors for acute respiratory tract infections in young Greenlandic children. Am J Epidemiol. 2003 Aug 15;158(4):374-84. doi: 10.1093/aje/kwg143.
Saeed AA, Bani IA. Prevalence and correlates of acute respiratory infections in children less than two years of age. Saudi Med J. 2000 Dec;21(12):1152-6.
Zaman K, Baqui AH, Yunus M, Sack RB, Bateman OM, Chowdhury HR, et al. Acute respiratory infections in children: a community-based longitudinal study in rural Bangladesh. J Trop Pediatr. 1997 Jun;43(3):133-7. doi: 10.1093/tropej/43.3.133.
Hajela, S. "Profile of Congenital Heart Disease in childhood." surgery 11 (2014): 12.
Cross TJ, Kim CH, Johnson BD, Lalande S. The interactions between respiratory and cardiovascular systems in systolic heart failure. J Appl Physiol (1985). 2020 Jan 1;128(1):214-224. doi: 10.1152/japplphysiol.00113.2019.
Gabriela, Krystle, Rahmat Budi Kuswiyanto, and Fenny Dwiyatnaningrum. "Clinical characteristic and outcome of acute lower respiratory tract infection in children with congenital heart disease." Althea Medical Journal 2.3 (2015): 403-408.
Cahyono, Agus, and Machrus A. Rachman. "The cause of mortality among congenital heart disease patients in Pediatric Ward, Soetomo General Hospital (2004-2006)." Indonesian Journal of Cardiology (2007): 279-284.
Wilar, Rocky, and J. M. Wantania. "Beberapa faktor yang berhubungan dengan episode infeksi saluran pernapasan akut pada anak dengan penyakit jantung bawaan." Sari Pediatri 8.2 (2016): 154-8.
Nataprawira, H. M., E. H. Alwi, and N. Adriani. "Faktor risiko morbiditas dan mortalitas pneumonia berat pada anak usia balita." Majalah Kedokteran Indonesia 60 (2010): 443-447.
Lanata CF, Rudan I, Boschi-Pinto C, Tomaskovic L, Cherian T, Weber M, et al. Methodological and quality issues in epidemiological studies of acute lower respiratory infections in children in developing countries. Int J Epidemiol. 2004 Dec;33(6):1362-72. doi: 10.1093/ije/dyh229.
Sommer C, Resch B, Simões EA. Risk factors for severe respiratory syncytial virus lower respiratory tract infection. Open Microbiol J. 2011;5:144-54. doi: 10.2174/1874285801105010144.
Fauroux B, Simões EAF, Checchia PA, Paes B, Figueras-Aloy J, Manzoni P, et al. The Burden and Long-term Respiratory Morbidity Associated with Respiratory Syncytial Virus Infection in Early Childhood. Infect Dis Ther. 2017 Jun;6(2):173-197. doi: 10.1007/s40121-017-0151-4.
Koch A, Mølbak K, Homøe P, Sørensen P, Hjuler T, Olesen ME, et al. Risk factors for acute respiratory tract infections in young Greenlandic children. Am J Epidemiol. 2003 Aug 15;158(4):374-84. doi: 10.1093/aje/kwg143.
Owayed AF, Campbell DM, Wang EE. Underlying causes of recurrent pneumonia in children. Arch Pediatr Adolesc Med. 2000 Feb;154(2):190-4. doi: 10.1001/archpedi.154.2.190.
Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002 Jun 19;39(12):1890-900. doi: 10.1016/s0735-1097(02)01886-7.
Nguyen TK, Tran TH, Roberts CL, Fox GJ, Graham SM, Marais BJ. Risk factors for child pneumonia - focus on the Western Pacific Region. Paediatr Respir Rev. 2017 Jan;21:95-101. doi: 10.1016/j.prrv.2016.07.002.
Zhang Q, Guo Z, Bai Z, MacDonald NE. A 4 year prospective study to determine risk factors for severe community acquired pneumonia in children in southern China. Pediatr Pulmonol. 2013 Apr;48(4):390-7. doi: 10.1002/ppul.22608.
Sadoh WE, Osarogiagbon WO. Underlying congenital heart disease in Nigerian children with pneumonia. Afr Health Sci. 2013 Sep;13(3):607-12. doi: 10.4314/ahs.v13i3.13.
Pongiglione G, Possidoni A, di Luzio Paparatti U, Costanzo AM, Gualberti G, Bonvicini M, et al. Incidence of Respiratory Disease During the First Two Years of Life in Children with Hemodynamically Significant Congenital Heart Disease in Italy: A Retrospective Study. Pediatr Cardiol. 2016 Dec;37(8):1581-1589. doi: 10.1007/s00246-016-1473-9.
Gabriela K, Kuswiyanto RB, Dwiyatnaningrum F. Clinical characteristic and outcome of acute lower respiratory tract infection in children with congenital heart disease. Althea Medical Journal. 2015 Sep 26;2(3):403-8.
Singh, Pankaj Kumar, Partha Kumar Chaudhuri, and A. K. Chaudhary. "Incidence of congenital heart disease in children with recurrent respiratory tract infection in tertiary hospital." IOSR Journal of Dental and Medical Science 16.9 (2017): 42-4.
Şahan, Yasemin Özdemir, Erhan Kılıçoğlu, and Zülal Ülger Tutar. "Evaluation of children with congenital heart disease hospitalized with the Diagnosis of Lower Respiratory Tract Infection." The Journal of Pediatric Research 5.1 (2018): 32.
Margolis P, Gadomski A. The rational clinical examination. Does this infant have pneumonia? JAMA. 1998 Jan 28;279(4):308-13. doi: 10.1001/jama.279.4.308.
Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015 Feb 26;372(9):835-45. doi: 10.1056/NEJMoa1405870.
Murphy CG, van de Pol AC, Harper MB, Bachur RG. Clinical predictors of occult pneumonia in the febrile child. Acad Emerg Med. 2007 Mar;14(3):243-9. doi: 10.1197/j.aem.2006.08.022.
Bachur R, Perry H, Harper MB. Occult pneumonias: empiric chest radiographs in febrile children with leukocytosis. Ann Emerg Med. 1999 Feb;33(2):166-73. doi: 10.1016/s0196-0644(99)70390-2.
Isaacs D. Problems in determining the etiology of community-acquired childhood pneumonia. Pediatr Infect Dis J. 1989 Mar;8(3):143-8.
Hageman JC, Uyeki TM, Francis JS, Jernigan DB, Wheeler JG, Bridges CB, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003-04 influenza season. Emerg Infect Dis. 2006 Jun;12(6):894-9. doi: 10.3201/eid1206.051141.
Frazee, Bradley W. "Update on emerging infections: news from the Centers for Disease Control and Prevention. Severe methicillin-resistant Staphylococcus aureus community-acquired pneumonia associated with influenza--Louisiana and Georgia, December 2006-January 2007." Annals of emergency medicine 50.5 (2007): 612-616.
Self WH, Williams DJ, Zhu Y, Ampofo K, Pavia AT, Chappell JD, et al. Respiratory Viral Detection in Children and Adults: Comparing Asymptomatic Controls and Patients With Community-Acquired Pneumonia. J Infect Dis. 2016 Feb 15;213(4):584-91. doi: 10.1093/infdis/jiv323.
Korppi M, Heiskanen-Kosma T, Kleemola M. Incidence of community-acquired pneumonia in children caused by Mycoplasma pneumoniae: serological results of a prospective, population-based study in primary health care. Respirology. 2004 Mar;9(1):109-14. doi: 10.1111/j.1440-1843.2003.00522.x.
Medrano C, Garcia-Guereta L, Grueso J, Insa B, Ballesteros F, Casaldaliga J, et al. Respiratory infection in congenital cardiac disease. Hospitalizations in young children in Spain during 2004 and 2005: the CIVIC Epidemiologic Study. Cardiol Young. 2007 Aug;17(4):360-71. doi: 10.1017/S104795110700042X.
Srinivasa, S., and Shruthi Patel. "A study on distribution pattern of lower respiratory tract infections in children under 5 years in a tertiary care centre." International Journal of Contemporary Pediatrics 5.2 (2018): 456.
Reddaiah, V. P., and S. K. Kapoor. "Acute Respiratory Infections In Underfives: Experience At Comprehensive Rural Health Services Project Hospital. Ballabgarh." Indian Journal of Community Medicine 20.2 (1995): 13.
Munagala VK, Mahesh RMU, Kandat J, Ponugoti M. Clinical study of lower respiratory tract infection in children attending a tertiary care hospital. Int J Contemp Pediatr. 2017;4:1733-8.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


