Clinicohematological profile of hemolytic anaemia in tertiary care hospital in rural Andhra Pradesh
Abstract
Introduction: Hemolytic anaemias are a group of disorders that cause significant morbidity in children.
Method: A cross sectional study was conducted at NRI Medical College for a period of 1 year. All cases of newly diagnosed and old cases of hemolytic anaemia on follow up were included.
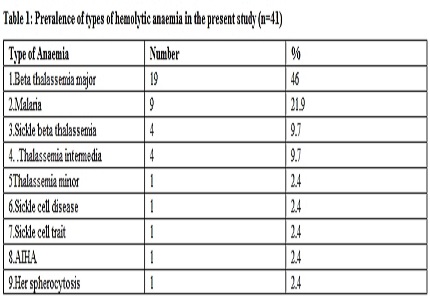
Results: The study showed beta thalassemia as the most common hemolytic anaemia; followed by malaria, sickle beta thalassemia, thalassemia intermedia, beta thalassemia minor, Sickle cell disease, sickle cell trait, auto immune hemolytic anaemia, and hereditary spherocytosis. The mean hemoglobin at presentation was 5.39 gm/dl. Anthropometric measurements in 32 cases of congenital hemolytic anaemias revealed height < 3rd centile in 9 cases. Weight less than 3rd centile was seen in 11 cases. 13 children had hemolytic facies. Massive splenomegaly causing discomfort, gall stones, heart failure were seen in 2 cases each. In thalassemia major, 10 cases required frequent transfusions, [10-12 per year]. 9 came for less frequent transfusions [6 per year]. Sickle thalassemia, thalassemia intermedia, required one transfusion every 1-2 years. Occasional transfusions were given in sickle cell anaemia, hereditary spherocytosis. Serum ferritin levels varied between 220-1427.
Conclusion: Hemoglobin electrophoresis remains the main investigation of choice in diagnosis of hemolytic anaemia. Thalassemia major is the most severe among other hemolytic anaemias encountered in this series. The study emphasizes the need to improve awareness regarding hemoglobinopathies among population, prenatal screening, blood transfusion policies, chelation policies to prevent complications in transfusion dependent patients.
Downloads
References
2. Weatherall DJ, Clegg JB: The thalassemia syndromes, 4th edition: Oxford Blackwell scientific publications;2001.
3. Surhone LM, Tennoe MTHenssonow SF, Congenital hemolytic anaemia, Saarbrucken, Germany: VDM Verlog, Dr.Muller ;2010.
4. UNICEF: The state of worlds children oxford: Oxford university press; 1996.
5. Yasish HM- Thalassemia: http://www.emedicine.com/PED/topic2229.htm; Accessed 23rd oct 2002.
6. Modell B, Berdoukas V. The clinical approach to Thalassemia: London:Gruns and Stration;1984.
7.La Nasa G, Caocci G, Argiolu F, Giardini C, Locatelli F, Vacca A, Orofino MG, Piras E, Addari MC, Ledda A, Contu L. Unrelated donor stem cell transplantation in adult patients with thalassemia. Bone marrow transplantation. 2005 Dec 1;36(11):971-5. [PubMed]
8. Verma IC, Choudhry VP, Jain PK. Prevention of thalassemia: a necessity in India. Indian journal of pediatrics. 1992 Nov 1;59(6):649-54. [PubMed]
9.Manglani M, Lokeshwar MR, Vani VG, Bhatia N, Mhaskar V. 'NESTROFT'--an effective screening test for beta thalassemia trait. Indian pediatrics. 1997 Aug;34(8):702-7. [PubMed]
10. Wild BJ, Bain BJ. Investigations of abnormal hemoglobins and thalassemia. In:Lews Sin, Bain BJ, Bates I, Dacie and Lewis practical hematology, 9th edition, London Curchill Livingstone:2001;231-68. [PubMed]
11. Balgir RS. The burden of hemoglobinopathies in India and the challenges ahead. Curr sci. 2000 Dec 10;79(11):1536-47.
12. Balgir RS. Spectrum of hemoglobinopathies in the state of Orissa, India: a ten years cohort study. JAPI. 2005 Dec;53:1021-6. [PubMed]
13Balgir RS. The genetic burden of hemoglobinopathies with special reference to community health in India and the challenges ahead. Indian J Hematol Blood Transfus. 2002;20(1):2-7.
14. Varawalla NY, Old JM, Sarkar R, Venkatesan R, Weatherall DJ. The spectrum of β‐thalassaemia mutations on the Indian subcontinent: the basis for prenatal diagnosis. British journal of haematology. 1991 Jun 1;78(2):242-7.
15. Shivashankara AR, Jailkhani R, Kini A. Hemoglobinopathies in Dharwad, North Karnataka: A hospital-based study. J Clin Diagnostic Res. 2008;2:593-9.
16. Preethi BP, Monika K, Maitreyee DS, Rashmi K. A hospital based study of Hereditary Hemolytic Anaemias in Davanagere district of Karnataka, India. Bangladesh journal of medical science. 2010 Jan 1;9(3):154.
17. Chattopadhyay K, Biswas R, Bhattacherjee S, Bandyopadhyay R. An epidemiological study on the clenico-hematological profile of patients with congenital hemolytic anemia in a tertiary care hospital of Kolkata. Indian J. Prev. Soc. Med. 2012 Oct;43(4):373.
18.Saxena A. Growth retardation in thalassemiaassemia major patients.Int .J .Human Genet .2003.3(4):237-46.
19. Grow K, Abrol P,Vasist M. Associated complications in beta thalassemia patients. IOSR Journal of pharmacy. 2013. Feb 3(1):22-25.
20. Tyagi S, Kabra M, Tandon N, Saxena R, Pati HP, Choudhry VP. Clinico-haematological profile of thalassemia intermedia patients. International Journal of Human Genetics. 2003;3(4):251.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


