Pattern of Early Neonatal Morbidities in Moderate and Late Pre-terms
Abstract
Objective: The present study is an attempt to analyze the data on the pattern of early neonatal morbidities among moderate and late preterm infants of 32 full weeks of gestation to 36+6 weeks’ gestational age in a tertiary care teaching hospital with a level III NICU, Chinna Kakani, A.P.
Materials and Methods: The study was a retrospective analysis of all live born preterms of 32+0– 36+6 GA, who were admitted between January, 2015 to April, 2016, over a period of 16 months. Data collected from hospital medical records of neonates were reviewed and analyzed statistically.
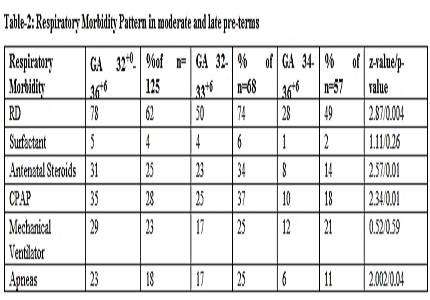
Results: Of total of 3067 deliveries conducted, 930 babies were admitted in NICU for various reasons. Of total admissions to NICU 125 (13%) infants were termed as moderate and late preterms after checking their GA and analyzed for the spectrum of early neonatal morbidities during their stay in hospital. Of total 125 babies, 58%(n=68) were moderate preterms and 45%(n=57) were late preterms, 75% (n=94) of them were AGA and 25%(n=32) were SGA. Of them, 62% (n=77) were delivered by LSCS while 38%(n=48) were delivered by NVD. Male infants comprised of 54% (n=67) while females were 46%(n=58). The mean weight at birth was 1.86 kg. Around 62% (n=78) of babies were observed for RD, of which 28% (n=35) required CPAP and 23%(n=29) for mechanical ventilation,18%(n=23) had apneas. Most common metabolic abnormality was hyper bilirubinemia at 44% (n=55) requiring phototherapy. Around 7% (N=9) received parenteral nutrition, NEC observed in 3%(n=3). Maternal co morbid conditions were associated in about 60% of cases.
Conclusion: Moderate preterms were significantly at a higher risk for over all morbidities, longer duration of hospital stays and at a high risk for mortality when compared to late preterms. Moderate and late preterm infants place high demands on specialist neonatal services.
Downloads
References
2.Howson CP, Kinney MV, McDougall L, Lawn JE; Born Too Soon Preterm Birth Action Group.Reprod Health. 2013;10 Suppl 1:S1. doi: 10.1186/1742-4755-10-S1-S1. Epub 2013 Nov 15. Review.PMID: 24625113. [PubMed]
3. Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C; GAPPS Review Group. Global report on preterm birth and stillbirth (1 of 7): definitions, descriptionof the burden and opportunities to improve data. BMC Pregnancy Childbirth. 2010 Feb 23;10 Suppl 1:S1. doi: 10.1186/1471-2393-10-S1-S1.PMID: 20233382. [PubMed]
4. Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical outcomes of near-term infants. Pediatrics. 2004 Aug;114(2):372–6. PMID: 15286219. [PubMed]
5. Howson CP, Kinney MV, McDougall L, Lawn JE; BornTooSoon Preterm Birth Action Group.Reprod Health. 2013;10 Suppl 1:S1. doi: 10.1186/1742-4755-10-S1-S1. Epub 2013 Nov 15. Review. PMID: 24625113. [PubMed]
6. Escobar GJ, Clark RH, Greene JD. Short-Term Outcomes of Infants Born at 35 and 36 Weeks Gestation: We Need to Ask More Questions. Semin Perinatol. 2006 Feb;30(1):28-33. Review.PMID: 16549211. [PubMed]
7. Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, Hoffman M, et al. Respiratory Morbidity in Late Preterm Births. JAMA. 2010 Jul 28;304(4):419-25. doi: 10.1001/jama.2010.1015.PMID: 20664042 . [PubMed]
8. Lawn JE, Mwansa-Kambafwile J, Horta BL, Barros FC, Cousens S. “Kangaroo mother care” to prevent neonatal deaths due to preterm birth complications. Int J Epidemiol. 2011 Apr;40(2):525-8.PMID: 21062786. [PubMed]
9. Khashu M, Narayanan M, Bhargava S, Osiovich H. Perinatal outcomes associated with preterm birth at 33 to 36 weeks’ gestation: apopulation-based cohort study. Pediatrics. 2009 Jan;123(1):109-13. doi: 10.1542/peds.2007-3743.PMID: 19117868.
10.Melamed N, Klinger G, Tenenbaum-Gavish K, Herscovici T, Linder N, Hod M, et al. Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Obstet Gynecol. 2009 Aug;114(2 Pt 1):253-60. doi: 10.1097/AOG.0b013e3181af6931.PMID: 19622985.
11. Young PC, Glasgow TS, Li X, Guest-Warnick G, Stoddard G. Mortality of late-preterm (near-term) newborns in Utah. Pediatrics. 2007 Mar;119(3):e659-65.PMID: 17332185. [PubMed]
12. Raju TNK, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics. 2006 Sep;118(3):1207-14.PMID: 16951017.
13. Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Weiss J, Evans S. Risk factors for neonatal morbidity and mortality among “healthy,” late preterm newborns. Semin Perinatol. 2006 Apr;30(2):54-60.PMID: 16731277. [PubMed]
14. Kirkby S, Greenspan JS, Kornhauser M, Schneiderman R. Clinical outcomes and cost of the moderately preterm infant. Adv Neonatal Care. 2007 Apr;7(2):80-7.PMID: 17605448. [PubMed]
15. Medoff Cooper B, Holditch‐Davis D, Terese Verklan M, Fraser‐Askin D, Lamp J, Santa‐Donato A, Onokpise B, Soeken KL, Bingham D.Newborn Clinical Outcomes of the AWHONN Late Preterm Infant ResearchBased Practice Project. J Obstet Gynecol Neonatal Nurs. 2012 Nov-Dec;41(6):774-85. doi: 10.1111/j.1552-6909.2012.01401.x. Epub 2012 Aug 3.PMID: 22861492.
16. Jaiswal A, Murki S, Gaddam P, Reddy A. Early neonatal morbidities in late preterm infants. IndianPediatr. 2011 Aug;48(8):607-11. Epub 2010 Nov 30.PMID: 21169647. [PubMed]
17. Pulver LS, Guest-Warnick G, Stoddard GJ, Byington CL, Young PC. Weight for gestational age affects the mortality of late preterm infants. Pediatrics. 2009 Jun;123(6):e1072-7. doi: 10.1542/peds.2008-3288. PMID: 19482740. [PubMed]
18. Black RE. Global Prevalence of Small for Gestational Age Births. Nestle Nutr Inst Workshop Ser. 2015;81:1-7. doi: 10.1159/000365790. Epub 2015 Jun 16.PMID: 26111558. [PubMed]
19. Kerstjens JM, Bocca-Tjeertes IF, de Winter AF, Reijneveld SA, Bos AF. Neonatal Morbidities and Developmental Delay in Moderately Preterm-Born Children. Pediatrics. 2012 Aug;130(2):e265-72.doi: 10.1542/peds.2012-0079. Epub 2012 Jul 9.PMID: 22778308. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


