Clinical study & laborotory profile of rickettsial fever in children- a study from rural Maharashtra
Abstract
Introduction: Rickettsial fever has been reported to be endemic in the Himalayan belt, Maharashtra and Karnataka in India among the adult population. Pediatric data on the same is limited in developing countries. Recently, the profile of rickettsial fever has been described in children in South India with similar clinical features.
Material Methods: This study was conducted from the patients admitted in our hospital, Ashwini Rural Medical College, Hospital & RC, Solapur, from the month of January 2014 to June 2015.The inclusion criteria were, clinical suspicion & supportive lab evidence – Weil Felix, positive leucocytosis, thrombocytopenia.
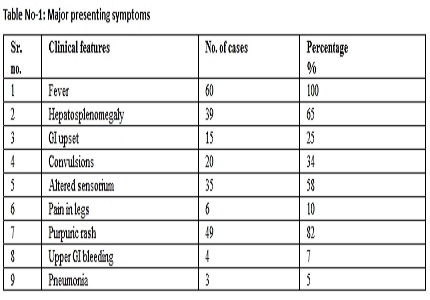
Results: In our study age of presentation ranged from 6 months to 12 years, with mean age of 7 yrs, there was no statistically significant sex difference. All patients presented with fever & purpuric rash was seen in 82%, altered sensorium was seen in 58 %, seizures were seen 34% & Hepatosplenomegaly was seen in 65 % of cases.
Other investigations: In our study CSF examination was done in 25 patients of which 10 had abnormal findings, 6 showed low sugar and 8 high protein. In our study according to the Weil Felix titers, most probable disease would be tick borne spotted fever or epidemic typhus, since no louse infestation (the scalp and body infestation, lymphadenopathy) was seen in any of the patients, and most of them were from rural areas more chances of tick infestation.
Conclusions: The diagnosis of rickettsia should always be kept in mind for workup of exanthematous fever. High index of clinical suspicion and good laboratory co- relation are helpful in detection of more no of cases. Early diagnosis and treatment with doxy and chloramphenicol can reduce the hospital stay and cost. Associated mixed infections may mislead diagnosis and are more fatal. Weil Felix test is not diagnostic standard. It should be interpreted in good clinical context, still it is easily available to all & remains good screening test.
Downloads
References
2. Ricketts HT. A micro-organism which apparently has a specific relationship to Rocky Mountain spotted fever. JAMA 1909;52: 379 –380. [PubMed]
3. Jensenius M, Fournier P, Raoult D. Rickettsioses and the international traveler. Clin Infect Dis. 2004;34(10):1493-9. [PubMed]
4. Helmick CG, Bernard KW, D'Angelo LJ. Rocky Mountain spotted fever: clinical, laboratory, and epidemiological features of 262 cases. J Infect Dis. 1984 Oct;150(4):480–488. [PubMed]
5. Padbidri VS, Gupta NP. Rickettsiosis in India: A review. J Indian Med Assoc 1978; 71: 104-107. [PubMed]
6. N. Murali, Swathi Pillai, Thomas Cherian, P. Raghupathy, V. Padmini, Elizabeth Mathai. Rickeetsial infections in South India: How to spot the spotted fever. Indian Pediatrics 2001; 38: 1393-1396. [PubMed]
7. Raoult D, Parola P, editors. Rickettsial Diseases. New York: Informa Healthcare USA 2007. [PubMed]
8. Frieden IJ, Resnick SD. Childhood exanthems – old and new. Pediatr Clin N Am. 1991; 38: 859-887. [PubMed]
9. Reller ME, Dumler SJ. Nelson text book of pediatric. 19th ed. Epidemic Typhus (Rickettsia prowazekii); 222.2: 1047-8.
10. Rathi N.,Rathi A. Indian Pediatrics: 2010 Feb;l47:159. [PubMed]
11. Colomba C, Laura S, Valentino FP, Raffaella R, Lucio T. Mediterranean spotted fever: clinical and laboratory characteristics of 415 Sicilian children. BMC Infect Dis. 2006;6: 60. [PubMed]
12. Nigwekar P, Kavar Y, Shrikhande DY, Ashok Kumar C. Clinico-pathological profile of Rickehsial Fever in a rural area of western Maharashtra, India. Pravara Med Rev. 2013;5(3):5-9.
13. Mahajan SK. Scrub typhus. J.Assoc. of Physic India. 2005;53:954-58. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


