Prevalence of microcytic hypocromic anemia in children with LRTI in the age group of 3 months to 5year: Is iron deficiency anemia a risk factor for LRTI?
Abstract
Introduction: Lower respiratory tract infection (LRTI) include all infections of the lungs and the large airways below the larynx and includes croup syndromes, bronchitis, bronchiolitis and pneumonia. Anemia is a major public health problem that can occur at any stage of the life cycle, but is more prevalent in pregnant women and young children having iron deficiency.
Methods: Objective: To evaluate prevalence of microcytic hypocromic anemia in children with LRTI in the age group of 3 months to 5 year: Is iron deficiency anemia a risk factor for LRTI.
Design: Cross sectional study.
Setting: A tertiary care center Karnataka, india (SIMS, shivamogga) Participants: 50 children who admitted for LRTI were included in the study group. Age and sex-matched 50 children, not having any respiratory illness, were taken as control group.
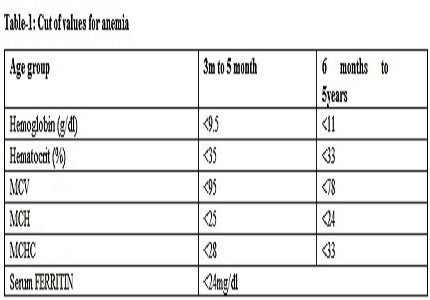
Main outcome measures: They were subjected to complete blood count (CBC) mainly for hemoglobin, hematocrite, RBC indices and RDW in those children.
Result: 35 out of 50 children of study group (70%) and 5 out of 50 children of control group (10%) had anemia. Out of 35 anemic children in study group 21(60%) and out of 5 anemic children in control group 4 had peripheral blood picture showing microcytic hypochromic anemia. And out of 35 anemic children in study group 28 (80%) and out of 5 anemic children in control group 2 had low ferritin.
Conclusion: these value shows anemia is more prevalent in children with LRTI and most of those anemic have microcytic hypochromic anemia with high RDW indicating iron deficiency is the cause for anemia and probably iron deficiency is a risk factor for LRTI.
Downloads
References
2. Chisti MJ, Tebruegge M, La Vincente S, Graham SM, Duke T. Pneumonia in severely malnourished children in developing countries - mortality risk, aetiology and validity of WHO clinical signs: a systematic review. Trop Med Int Health. 2009 Oct;14(10):1173-89. doi: 10.1111/j.1365-3156.2009.02364.x.
3. Bruno de Benoist, Erin McLean, Ines Egli and Mary Cogswell. Worldwide prevalence of anaemia 1993–2005 : WHO global database on anaemia. World Health Organization 2008//: [accessed on 25/8/2013]
4. Pasricha SR, Black J, Muthayya S, Shet A, Bhat V, Nagaraj S, Prashanth NS, Sudarshan H, Biggs BA, Shet AS. Determinants of anemia among young children in rural India. Pediatrics. 2010 Jul;126(1):e140-9. doi: 10.1542/peds.2009-3108. Epub 2010 Jun 14.
5. Malla T, Pathak OK, Malla KK. Is Low Hemoglobin level a risk factor for acute lower respiratory tract infections?J Nepal Pediatric Soci.2010;30:1–7.
6. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity VMNIS | Vitamin and Mineral Nutrition Information System WHO/NMH/NHD/MNM/11.1
7. Vinod k Paul, Arvind Bagga, Adithi Sinha: O P Ghai 8th edition: CBC publishers : p 330 – 337.
8. Hermiston ML, Mentzer WC. A practical approach to the evaluation of the anemic child. Pediatr Clin North Am. 2002 Oct;49(5):877-91. [PubMed]
9. Beutler E, Waalen J. The definition of anemia: what is the lower limit for normal of the blood hemoglobin concentration. Blood. 2006;5:1747–1750. [PubMed]
10. Bhaskaram P, Madhavan Nair K, Balakrishna N, Ravinder P, Sesikeran B. Serum transferrin receptor in children with respiratory infections. Eur J Clin Nutr. 2003 Jan;57(1):75-80. [PubMed]
11. de Silva A, Atukorala S, Weerasinghe I, Ahluwalia N. Iron supplementation improves iron status and reduces morbidity in children with or without upper respiratory tract infections: a randomized controlled study in Colombo, Sri Lanka. Am J Clin Nutr. 2003 Jan;77(1):234-41. [PubMed]
12. Forssell G, Håkansson A, Månsson NO. Risk factors for respiratory tract infections in children aged 2-5 years. Scand J Prim Health Care. 2001 Jun;19(2):122-5.
13. Koch A, Molbak K, Homoe P, Sorensen P, Hjuler T, Olessen ME et al. Risk factors for acute respiratory tract infections in young Greenlandic children. Am J Epidemiol 2003; 158: 374-384.
14. William F Ganong. Gas transport between the lungs and the tissues. Review of Medical Physiology. 22nd ed. New York; Mc Graw-Hill, 2005: 666-669.
15. Guyton & Hall. Effect of hemoglobin to ‘Buffer’ the tissue PO2. Text Book of Medical Physiology. 11th ed. Philadelphia; Saunders, 2006: 507-508.
16. Hussain, Sheikh Quyoom, et al. Low hemoglobin level a risk factor for acute lower respiratory tract infections (ALRTI) in children. Journal of clinical and diagnostic research: JCDR 8.4 (2014): PC01.
17. Malla T, Pathak OK, Malla KK. Is low haemoglobin level a risk factor for lower respiratory tract infection. Indian J Pediatr. 2006;73:881–3.
18. Mourad S, Rajab M, Alameddine A, Fares M, Ziade F, Merhi BA. Hemoglobin level as a risk factor for lower respiratory tract infections in Lebanese children. N Am J Med Sci. 2010 Oct;2(10):461-6. doi: 10.4297/najms.2010.2461.
19. Ramakrishnan K, Harish PS. Hemoglobin level as a risk factor for lower respiratory tract infections. Indian J Pediatr. 2006 Oct;73(10):881-3. [PubMed]
20. National heart, lung, blood institute: what causes anemia. https://www.nhlbi.nih.gov/health/health-topics/topics/anemia/causes[accessed on 25/8/2013] [PubMed]
Copyright (c) 2014 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


