Oxygen saturation trend and comparison between oxygen saturation levels in normal delivered and caserean section delivered babies within 30 minutes of life
Abstract
Objective: To determine normal arterial oxygen saturation (SpO2) trend during first 30 min of life and to evaluate for difference in SpO2 trends in healthy term newborns of normal delivered (NVD) and caserean section (CS) and to determine the possible relationship between the normal levels of oxygen saturation and birth weight at 0 and 5th minute of life.
Methods: This Prospective Cross-sectional Observational study was conducted in Department of Paediatric Medicine SMS Medical College, Jaipur. Term neonates born by NVD and elective CS were included and readings of oxygen saturation levels were obtained at an interval of 5 minutes up to 30 minutes. Secondary objective is to determine the relation of SpO2 levels of term newborn with birth weight irrespective of mode of delivery.
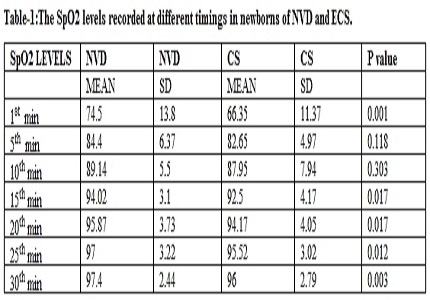
Results: Difference in values of NVD and CS neonates were statistically significant for 1st and 30th min (p- 0.001 and -0.003) respectively. SpO2 is negatively related to birth weight.
Conclusions: The study defines the normal SpO2 in healthy term newborns of NVD and CS and also concludes that there is significant difference in SpO2 levels at 1st and 30th minute of life in NVD and CS babies. In healthy term newborns, levels of SpO2 measured at 1st and 5th minute of life are negatively related to birth weight.
Downloads
References
2. East C E, Colditz P B, Begg L M. et al Update on intrapartum fetal pulse oximetry. Aust N Z J Obstet Gynaecol 200242119–124.124. [PubMed]
3. International Liaison Committee on Resuscitation. 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 7: Neonatal resuscitation. Resuscitation. 2005 Nov-Dec;67(2-3):293-303.
4. Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010 Oct;81(10):1219-76. doi: 10.1016/j.resuscitation.2010.08.021. [PubMed]
5. Dawson JA, Davis PG, O'Donnell CP, Kamlin CO, Morley CJ. Pulse oximetry for monitoring infants in the delivery room: a review. Arch Dis Child Fetal Neonatal Ed. 2007 Jan;92(1):F4-7. [PubMed]
6. Kattwinkel J. Evaluating resuscitation practices on the basis of evidence: the findings at first glance may seem illogical. J Pediatr. 2003 Mar;142(3):221-2.
6. American Heart Association American Heart Association (AHA) Guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: neonatal resuscitation guidelines. Pediatrics 20061171029–1038.1038.
7. Leone T A, Finer N N. Neonatal resuscitation: beyond the basics. NeoReviews 20056e177–e183.e183.
8. Leone TA, Rich W, Finer NN. A survey of delivery room resuscitation practices in the United States. Pediatrics. 2006 Feb;117(2):e164-75. [PubMed]
9. Hay WW Jr, Brockway JM, Eyzaguirre M. Neonatal pulse oximetry: accuracy and reliability. Pediatrics. 1989 May;83(5):717-22. [PubMed]
10. Harris A P, Sendak M J, Donham R T. Changes in arterial oxygen saturation immediately after birth in the human neonate. J Pediatr 1986109117–119.119. [PubMed]
11. Hulsoore R, Shrivastav J, Dwivedi R. Normal oxygen saturation trend in healthy term newborns within 30 minutes of birth. Indian J Pediatr. 2011 Jul;78(7):817-20. doi: 10.1007/s12098-011-0405-1. Epub 2011 Mar 17.
12. Zubarioglu U, Uslu S, Can E, Bülbül A, Nuhoglu A. Oxygen saturation levels during the first minutes of life in healthy term neonates. Tohoku J Exp Med. 2011;224(4):273-9. [PubMed]
13. House JT, Schultetus RR, Gravenstein N. Continuous neonatal evaluation in the delivery room by pulse oximetry. J Clin Monit. 1987 Apr;3(2):96-100. [PubMed]
14. Meier‐Stauss P, Bucher H U, Hürlimann R. et al Pulse oximetry used for documenting oxygen saturation and right‐to‐left shunting immediately after birth. Eur J Pediatr 1990149851–855.855 [PubMed]
15. Røsvik A, Øymar K, Kvaløy JT, Berget M. Oxygen saturation in healthy newborns; influence of birth weight and mode of delivery. J Perinat Med. 2009;37(4):403-6. doi: 10.1515/JPM.2009.070. [PubMed]
16. Rabi Y, Yee W, Chen SY, Singhal N. Oxygen saturation trends immediately after birth. J Pediatr. 2006 May;148(5):590. [PubMed]
17. Kopotic RJ, Lindner W. Assessing high-risk infants in the delivery room with pulse oximetry. Anesth Analg. 2002 Jan;94(1 Suppl):S31-6. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


