Antibiotic susceptibility of bacterial agents in children with SAM: A single-centre cross-sectional study
Abstract
Purpose: To evaluate bacterial and fungal infections, and antibiotic sensitivity in children with severe acute malnutrition.
Methods: Design: Cross-sectional study.
Setting: Severe Malnutrition Treatment Unit of Pediatric ward of a tertiary level hospital attached to a medical college located in Rewa, Madhya Pradesh, India.
Participants: 100 Children with severe acute malnutrition aged 6-59 months. Blood, urine, CSF (cerebrospinal fluid) and pleural fluid samples were cultured and antibiotic sensitivity pattern determined.
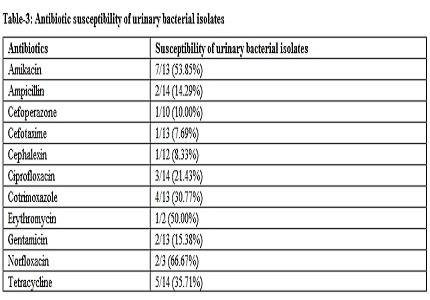
Results: Blood and urine culture were positive in 28 (28%) and 16 (16%), respectively, CSF and pleural fluid culture were positive in 12.5% (1 out of 8) and 100% (1 out of 1) cases, respectively. Gram-positive bacteria constitute 25 (56.82%) of the total bacterial isolates, where Staphylococcus aureus was most common while Escherichia coli was leading gram-negative bacteria. Blood culture showed 78.57% gram-positive bacteria predominantly coagulase-negative staphylococcus (28.57%), S. aureus (25%) and Enterococcus (25%). Gram-negative blood bacterial isolates constitute equal proportions of E. coli and Klebsiella 10.71% each. Urine bacterial isolates constitute predominantly E. Coli (64.29%) followed by Klebsiella (21.43%). Bacterial isolates showed high level of susceptibility to amikacin (76.19%) followed by tetracycline (57.14%) and gentamcin (44.19%). Low level of susceptibility was observed to ampicillin (11.36%), ciprofloxacin (16.67%) and co-trimoxazole (20.59%).
Conclusions: Bacteraemia affected 28% children with severe acute malnutrition predominantly gram-positive isolates. Urine culture was dominated by gram-negative bacteria mostly E. Coli. Most bacterial isolates were resistant to commonly used antibiotics. Current guidelines for antibiotic of choice need to be reviewed.
Downloads
References
2. Ikeogu MO Wolf B, Mathe S. Pulmonary manifestations in HIV seropositivity and malnutrition in Zimbabwe. Arch Dis Child. 1997 Feb;76(2):124-8. [PubMed]
3. Mondal D, Haque R, Sack RB, Kirkpatrick BD, Petri WA Jr. Attribution of malnutrition to cause-specific diarrheal illness: evidence from a prospective study of preschool children in Mirpur, Dhaka, Bangladesh. Am J Trop Med Hyg. 2009 May;80(5):824-6.
4. Khatun F, Faruque AS, Koeck JL, Olliaro P, Millet P, Paris N, Malek MA, Salam MA, Luby S. Changing species distribution and antimicrobial susceptibility pattern of Shigella over a 29-year period (1980–2008). Epidemiol Infect 2011 Mar;139(3): 446-52. doi: 10.1017/S0950268810001093. Epub 2010 May 18.
5. Berkley JA, Lowe BS, Mwangi I, Williams T, Bauni E, Mwarumba S, Ngetsa C, Slack MP, Njenga S, Hart CA, Maitland K, English M, Marsh K, Scott JA. Bacteremia among children admitted to a rural hospital in Kenya. N Engl J Med. 2005 Jan 6;352(1):39-47. [PubMed]
6. Aiken AM, Mturi N, Njuguna P, Mohammed S, Berkley JA, Mwangi I, Mwarumba S, Kitsao BS, Lowe BS, Morpeth SC, Hall AJ, Khandawalla I, Scott JA; Kilifi Bacteraemia Surveillance Group. Risk and causes of paediatric hospital-acquired bacteraemia in Kilifi District Hospital, Kenya: a prospective cohort study. Lancet. 2011 Dec 10;378(9808):2021-7. doi: 10.1016/S0140-6736(11)61622-X. Epub 2011 Nov 29. [PubMed]
7. WHO Multicentre Growth Reference Study Group. WHO child growth standards: methods and development. Growth velocity based on weight, length and head circumference. Geneva: World Health Organization; 2009 (www.who.int/childgrowth/standards/velocity/technical_report/en/index.html, accessed 30 August 2013)
8. Hill PC, Onyeama CO, Ikumapayi UN, Secka O, Ameyaw S, Simmonds N, Donkor SA, Howie SR, Tapgun M, Corrah T, Adegbola RA. Bacteraemia in patients admitted to an urban hospital in West Africa. BMC Infectious Dis. 2007 Jan 26;7:2. [PubMed]
9. Ekanem EE, Umotong AB, Raykundalia C, Catty D. Serum C-reactive protein and C3 complement protein levels in severely malnourished Nigerian children with and without bacterial infections. Acta Paediatrica. 1997 Dec;86(12):1317–20.
10. Babirekere-Iriso E, Musoke P, Kekitiinwa A. Bacteraemia in severely malnourished children in an HIV-endemic setting. Ann Trop Paediatr. 2006 Dec;26(4):319–28. [PubMed]
11. Bachou H, Tylleskar T, Kaddu-Mulindwa DH, and Tumwine JK. “Bacteraemia among severely malnourished children infected and uninfected with the human immunodeficiency virus-1 in Kampala, Uganda. BMC Infectious Dis. 2006 Nov 7;6:160.
12. Noorani N, Macharia WM, Oyatsi D, Revathi G. Bacterial isolates in severely malnourished children at Kenyatta National Hospital, Nairobi. East Afr Med J. 2005 Jul;82(7):343–8.
13. Friedland IR. Bacteraemia in severely malnourished children. Ann Trop Paediatr. 1992;12(4):433-40. [PubMed]
14. Reed RP, Wegerhoff FO, Rothberg AD. Bacteraemia in malnourished rural African children. Ann Trop Paediatr. 1996 Mar;16(1):61-8. [PubMed]
15. Christie CD, Heikens GT, Golden MH. Coagulase-negative staphylococcal bacteremia in severely malnourished Jamaican children. Pediatr Infect Dis J. 1992 Dec;11(12):1030-6.
16. von Eiff C, Peters G, Heilmann C. Pathogenesis of infections due to coagulase-negative staphylococci. Lancet Infect Dis. 2002 Nov;2(11):677-85.
17. Rabasa AI, Shattima D. Urinary tract infection in severely malnourished children at the University of Maiduguri Teaching Hospital. J Trop Pediatr. 2002 Dec;48(6):359-61.
18. Reed RP and Wegerhoff FO. Urinary tract infection in malnourished rural African children. Ann Trop Paediatr. 1996 Mar;16(1):61-8. [PubMed]
19. Banapurmath CR and Jayamony S. Prevalence of urinary tract infection in severely malnourished preschool children. Indian Pediatr. 1994 Jun;31(6):679-82. [PubMed]
20. Blomberg B, Manji KP, Urassa WK, Tamim BS, Mwakagile DS, Jureen R, Msangi V, Tellevik MG, Holberg-Petersen M, Harthug S, Maselle SY, Langeland N. Antimicrobial resistance predicts death in Tanzanian children with bloodstream infections: a prospective cohort study. BMC Infect Dis. 2007 May 22;7:43.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


