A prospective seroepidemiologic study on dengue in children in Southeastern Rajasthan, India
Abstract
Background: In India, dengue epidemics are becoming more frequent (WHO, 2008). The majority of dengue viral infections are self-limiting, but complications may cause high morbidity and mortality.
Objectives: To assess the clinical profile of the dengue infection in children less than 18 years of age and to evaluate the outcomes of dengue fever from July2015 to June 2016 at Pediatric Department of J.K. Lon Hospital, Government Medical College, Kota the largest tertiary care hospital of southeastern Rajasthan.
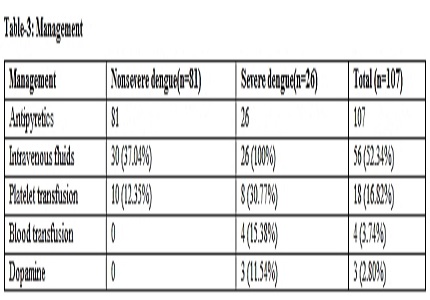
Results: A total of 107 cases were classified into 81 (75.70%) nonsevere and 26(24.30%) severe dengue cases. The most common age of presentation was above 11 yrs. The mean age of admission was 8.9 yrs. The most common presenting symptom was fever seen in 100% cases and hepatomegaly (22.06%) was the most common physical finding. Elevation in aspartate transaminase (SGOT) was found in 28.03% and thrombocytopenia in 52.30%. The correlation between hepatomegaly and elevated SGOT was significant (value 0.0346). Case fatality rate (CFR) was 0 %. The mean duration of hospitalization was 5.2 days.
Conclusion: In children, if symptoms like fever, pain, rashes, and vomiting are associated with hepatomegaly and elevated SGOT in context of low platelet count, a strong possibility of dengue fever is present, especially in an epidemic setting. Early suspicion and effective management can reduce the severity.
Downloads
References
2. Special Programme for Research, Training in Tropical Diseases, and World Health Organization,Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control, World Health Organization, Geneva, Switzerland, 2009.
3. N. Gupta, S. Srivastava, A. Jain, and U. C. Chaturvedi. Dengue in India. Indian Journal of Medical Research. 136(3),2012:373–90. [PubMed]
4. B. Das, M. Das, B. Dwibedi, S. K. Kar, and R. K. Hazra. Molecular investigations of dengue virus during outbreaks in Orissa state, Eastern India from 2010 to 2011. Infection, Genetics and Evolution, 16, 2013;401–10.
5. Rigau-Pérez JG, Clark GG, Gubler DJ, Reiter P, Sanders EJ, Vorndam AV. Dengue and dengue haemorrhagic fever. Lancet. 1998 Sep 19;352(9132):971-7. [PubMed]
6. World Health Organization, WHO report on global surveillance of Epidemic prone infectious diseases. http://apps.who.int/iris/bitstream/10665/66485/1/WHO_CDS_CSR_ISR_2000.1.pdf.
7. O. Wichmann, S. Hongsiriwon, C. Bowonwatanuwong, K. Chotivanich, Y. Sukthana, and S. Pukrittayakamee. Risk factors and clinical features associated with severe dengue infection in adults and children during the 2001 epidemic in Chonburi, Thailand. Tropical Medicine & International Health, 9(9)2004;1022–9.
8. S. Padhi, M. Dash, P. Panda et al. A three year retrospective study on the increasing trend in seroprevalence of dengue infection from southern Odisha, India. The Indian Journal of Medical Research;140,2014;660–4.
9. Basuki PS, Budiyanto, Puspitasari D, Husada D, Darmowandowo W, Ismoedijanto, Soegijanto S, Yamanaka A. Application of revised dengue classification criteria as a severity marker of dengue viral infection in Indonesia. Southeast Asian J Trop Med Public Health. 2010 Sep;41(5):1088-94. [PubMed]
10. S. Ahmed, F. Arif, Y. Yahya et al. Dengue fever outbreak in Karachi 2006-a study of profile and outcome of children under 15 years of age. Journal of the Pakistan Medical Association,58(1),2008; 4–8. [PubMed]
11. Joshi R, Baid V. Profile of dengue patients admitted to a tertiary care hospital in Mumbai. Turk J Pediatr. 2011 Nov-Dec;53(6):626-31. [PubMed]
12. H. Mittal, M. M. A. Faridi, S. K. Arora, and R. Patil. Clinicohematological profile and platelet trends in children with dengue during 2010 epidemic in North India. Indian Journal of Pediatrics, 79(4), 2012; l467–471.
13. C. Krishnamurti, S. Kalayanarooj, M. A. Cutting et al. Mechanisms of hemorrhage in dengue without circulatory collapse. American Journal of Tropical Medicine and Hygiene, 65(6), 2001; 840–847.
14. Kalayanarooj S, Vaughn DW, Nimmannitya S, Green S, Suntayakorn S, Kunentrasai N, Viramitrachai W, Ratanachu-eke S, Kiatpolpoj S, Innis BL, Rothman AL, Nisalak A, Ennis FA. Early clinical and laboratory indicators of acute dengue illness. J Infect Dis. 1997 Aug;176(2):313-21. [PubMed]
15. Ratageri VH, Shepur TA, Wari PK, Chavan SC, Mujahid IB, Yergolkar PN. Clinical profile and outcome of Dengue fever cases. Indian J Pediatr. 2005 Aug;72(8):705-6. [PubMed]
16. I. Shah and B. Katira. Clinical and laboratory abnormalities due to dengue in hospitalized children in Mumbai in 2004. Dengue Bulletin;29;2005; 90–96.
17. K. Wanigasuriya, P. Gurugama, A. Wijewickrama, S. L. Seneviratne, and S. B. Gunatilake. Usefulness of World Health Organization (WHO) dengue case classifications in a Sri Lankan clinical setting. Journal of the Ceylon College of Physicians, 42(1-2), 2012;21–27.
18. S. L. Seneviratne, G. N. Malavige, and H. J. de Silva, Pathogenesis of liver involvement during dengue viral infections. Transactions of the Royal Society of Tropical Medicine and Hygiene, 2006;100(7): 608–614.
19. Ghosh A, Dar L. Dengue vaccines: challenges, development, current status and prospects. Indian J Med Microbiol. 2015 Jan-Mar;33(1):3-15. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


