Effect of surfactant therapy using an orogastric tube for tracheal catheterization in preterm newborns with respiratory distress
Abstract
Introduction: Respiratory distress syndrome (RDS) due to surfactant deficiency requires surfactant therapy for which InSurE method (Intubate, Surfactant, Extubate) has been widely used. However this method requires intubation and positive pressure ventilation, even for a short time which is enough to initiate significant lung injury. Recently, surfactant administration by Minimally Invasive Surfactant Therapy (MIST) using a fine catheter under direct laryngoscopy in spontaneously breathing preterms while on nCPAP has reported good outcomes. We prospectively assessed the outcome of a modified MIST method of surfactant administration using an orogastric tube in preterms with RDS.
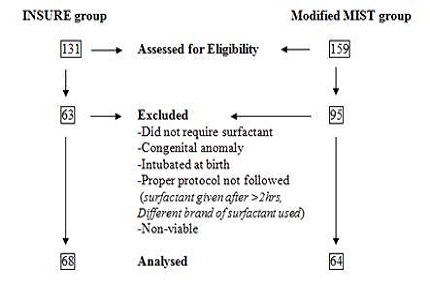
Materials & Methods: A single centre, prospective observational study was conducted where all consecutive eligible inborn preterm neonates with gestation age more than 24 weeks but less than 34 weeks and suffering from RDS were enrolled to receive surfactant using MIST. Results were compared with a historical cohort of preterm who received surfactant with INSURE techniques.
Results: Sixty four cases in the modified MIST group were compared with a historic cohort of 68 cases in INSURE group. There were no differences in the requirement of intubation and mechanical ventilation in the first 72 hours but the duration of MV and CPAP were significantly less in modified MIST group. Other neonatal morbidities and mortality rates were similar in either of the groups.
Conclusion: The modified MIST technique is an effective method for the treatment of RDS in preterms with better clinical efficacy and comparable outcomes than the more invasive INSURE procedure and deserves further evaluation.
Downloads
References
2. Public Health Foundation of India, All India Institute of Medical Sciences, Save the Children. Zodpey S, Paul VK, editors. State of India’s Newborns (SOIN) 2014- A Report. New Delhi: PHFI, AIIMS, SC;2014. [PubMed]
3. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sánchez PJ, O'Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID 3rd, Watterberg KL, Saha S, Das A, Higgins RD; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010 Sep;126(3):443-56. doi: 10.1542/peds.2009-2959. Epub 2010 Aug 23.
4. Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrøm K, Jacobsen T. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicentre Study Group. N Engl J Med. 1994 Oct 20;331(16):1051-5.
5. Björklund L, Ingimarsson J, Curstedt T, Johan J, Robertson B, Werner O et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatric Research. 1997;42(3):348–355. DOI:10.1203/00006450-199709000-00016.
6. Kribs A, Pillekamp F, Hünseler C, Vierzig A, Roth B. Early administration of surfactant in spontaneous breathing with nCPAP: Feasibility and outcome in extremely premature infants (postmenstrual age d”27 weeks). Paediatr Anaesth. 2007;17:364-9. [PubMed]
7. Silverman WC, Anderson DH. Controlled clinical trial on effects of water mist on obstructive respiratory signs, death rate and necropsy findings among premature infants. Pediatrics 1956; 17: 1-4.
8. Kliegman RM, Walsh MC. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr. 1987 Apr;17(4):213-88.
9. International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005 Jul;123(7):991-9. [PubMed]
10. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978 Apr;92(4):529-34. [PubMed]
11. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001 Jun;163(7):1723-9. [PubMed]
12. Göpel W, Kribs A, Ziegler A, Laux R, Hoehn T, Wieg C, et al. German Neonatal Network. Avoidance of mechanical ventilation by surfactant treatment of spontaneously breathing preterm infants (AMV): an open-label, randomised, controlled trial. Lancet. 2011;378(9083):1627-34. DOI: 10.1016/S0140-6736(11)60986-0. [PubMed]
13. Kribs A, Härtel C, Kattner E, Vochem M, Küster H, Möller J, et al. Surfactant without intubation in preterm infants with respiratory distress: First multi-center data. Klin Padiatr. 2010;222:13-7. DOI: 10.1055/s-0029-1241867.
14. Kanmaz HG, Erdeve O, Canpolat FE, Mutlu B, Dilmen U. Surfactant Administration via thin catheter during spontaneous breathing: Randomized controlled trial. Pediatrics. 2013;131(2):e502-9. DOI: 10.1542/peds.2012-0603.
15. Aguar M, Cernada M, Brugada M, Gimeno A, Gutierrez A, Vento M. Minimally invasive surfactant therapy with a gastric tube is as effective as the intubation, surfactant, and extubation technique in preterm babies. Acta Paediatr. 2014 Jun;103(6):e229-33. doi: 10.1111/apa.12611. Epub 2014 Mar 15.
16. Yost CC, Soll RF. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev. 2000;(2): CD001456. [PubMed]
17. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, Yoder BA, Faix RG, Das A, Poole WK, Donovan EF, Newman NS, Ambalavanan N, Frantz ID 3rd, Buchter S, Sánchez PJ, Kennedy KA, Laroia N, Poindexter BB, Cotten CM, Van Meurs KP, Duara S, Narendran V, Sood BG, O'Shea TM, Bell EF, Bhandari V, Watterberg KL, Higgins RD. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010 May 27;362(21):1970-9. doi: 10.1056/NEJMoa0911783. Epub 2010 May 16.
18. Dunn MS, Kaempf J, de Klerk A, de Klerk R, Reilly M, Howard D, Ferrelli K, O'Conor J, Soll RF; Vermont Oxford Network DRM Study Group. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics. 2011 Nov;128(5):e1069-76. doi: 10.1542/peds.2010-3848. Epub 2011 Oct 24.
19. Sandri F, Plavka R, Ancora G, Simeoni U, Stranak Z, Martinelli S, et al. CURPAP Study Group. Prophylactic or early selective surfactant combined with nCPAP in very preterm infants. Pediatrics. 2010;125(6):e1402-9. DOI:10.1542/peds.2009-2131.
20. Petrikovsky BM, Lysikiewicz A, Markin LB, Slomko Z. In utero surfactant administration to preterm human fetuses using endoscopy. Fetal Diagnosis Therapy. 1995; 10(2): 127-30.
21. Berggren E, Liljedahl M, Winbladh B, et al. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Paediatr. 2000;89(4):460-4. [PubMed]
22. Kattwinkel J, Robinson M, Bloom BT Delmore P, Ferguson JE. Technique for intrapartum administration of surfactant without requirement for an endotracheal tube. J Perinatol. 2004; 24(6):360-365.
23. Attridge JT, Stewart C, Stukenborg GJ, Kattwinkel J. Administration of rescue surfactant by laryngeal mask airway: lessons from a pilot trial. Am J Perinatol. 2013(3); 30:201-6. DOI:10.1055/s-0032-1323592. [PubMed]
24. Dargaville PA, Aiyappan A, Cornelius A, Williams C, De Paoli AG. Preliminary evaluation of a new technique of minimally invasive surfactant therapy. Arch Dis Child Fetal Neonatal Ed. 2011;96(4): F243–8. DOI:10.1136/adc.2010.192518. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


