Hearing loss in high risk neonates
Abstract
Objective: To determine the incidence and risk factors associated with hearing loss in high risk neonates.
Design: Descriptive cross sectional study.
Setting: Level II NICU of a tertiary care hospital.
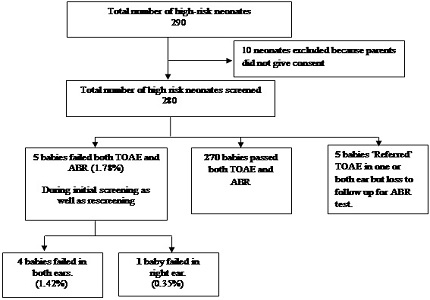
Participants: 280 high risk infants were screened.
Intervention: All high-risk babies were initially screened with both transient evoked otoacoustic emissions (TOAE) and Auditory brainstem response (ABR).
Outcome variables:
Primary: to determine the incidence of auditory neuropathy in high risk infants;
Secondary: risk factors in those babies identified with hearing loss.
Results: Incidence of hearing loss was 17.8 per 1000 screened (95% C.I is 0.24% - 3.32%), with bilateral hearing loss seen in 14.2 per 1000 babies. Highest incidence of hearing loss was seen is in infants with intracranial haemorrhage and meningitis (50%) followed by in decreasing orders craniofacial anomalies (20%), intrauterine congenital infections (11.11%), culture positive sepsis including meningitis (8.88%), birth weight less than 1.5 kg (7.14%), preterm < 33 weeks (4.34%), severe birth asphyxia (4%), use of ototoxic medications for more than 5 days (3.03%). The risk of hearing loss is higher with higher number of risk factors. With a single risk factor being present, it is only 0.66%, whereas with five risk factors, the incidence was 33.3%.
Conclusion: There is a high incidence of hearing loss in at-risk infants. Hearing loss is commoner when risk factors such as intracranial haemorrhage or meningitis are present and with presence of multiple risk factors. This would justify the need to routinely screen all high risk infants, so that rehabilitative measures can be initiated at the earliest.
Downloads
References
2. Paul Abraham K. Early Identification of Hearing Loss and Centralized Newborn Hearing Screening Facility-The Cochin Experience. Indian Pediatrics 2011;48: 355-359.
3. Nagapoornima P, A Ramesh, Srilakshmi, Rao Suman, Patricia P L, Gore Madhuri et al. Universal Hearing Screening. Indian J Pediatr 2007; 74 (6) : 545-9.
4. Evidence based clinical practice guidelines. National Neonatology Forum, India. October 2010.p. 265-270.
5. Joint Committee on Infant hearing (1994) Position statement. ASHA 36:38-41. [PubMed]
6. Joint Committee on Infant Hearing Position Statement. Pediatrics 2007; 120 (4): 898-921. [PubMed]
7. Joint Committee on Infant Hearing (JCIH) Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. Pediatrics 2000; 106 (4): 798-817.
8. Jewel John, Varghese P V, Singh Tejinder, Varghese Ashish. Newborn Hearing Screening—Experience at a Tertiary Hospital in Northwest India. International Journal of Otolaryngology and Head & Neck Surgery 2013, 2: 211-214.
9. Sudhir Rughani, Bhadresh Vyas, Vikas Sinha, Maulik Shah, Yamini Kapileshwarkar, Sonal Shah. Hearing screening in new born (A cross-sectional study). World Articles in Ear, Nose and Throat 2011; Volume 4 (1). http://waent.org/archives/2011/Vol4-1/20110515.HearingScreening/otoacoustic-emissions.htm accessed on 16.11.2011.
10. Kumar Anil YC, Chandrashekar and Sodhi Kirandeep. Universal Hearing Screening In Newborn. International Journal of Basic and Applied Medical Sciences 2013; 3 (2): 116-121.
11. Flynn Mark, Austin Nicola, Flynn Traci Schmidtke, Ford Rodney, Buckland Liz. Universal Newborn Hearing Screening introduced to NICU infants in Canterbury Province, New Zealand. Journal of the New Zealand Medical Association 2004; Vol 117 No 1206.
12. Khaimook Wandee, Chayarpham Satit, Dissaneevate Supaporn. The High-Risk Neonatal Hearing Screening Program in Songklanagarind Hospital. J Med Assoc Thai 2008; 91 (7): 1038-1042.
13. Basar Figen, Gul Guven Ayse. The Distribution of Risk Factors among High Risk Infants Who Failed at Hearing Screening. The Mediterranean Journal of Otology 2008; 211-216. [PubMed]
14. Ur Rehman M, Mando K, Rahmani A, Imran A, Ur Rehman N, Gowda K, Chedid F. Screening for neonatal hearing loss in the Eastern region of United Arab Emirates. East Mediterr Health J. 2012 Dec;18(12):1254-6. [PubMed]
15. Liu Z, Liu L. Hearing screening and diagnosis in a large sample of infants in Central China. J Med Screen. 2013 Mar;20(1):21-6. doi: 10.1177/0969141313478002. Epub 2013 May 13. [PubMed]
16. Taghdiri Mohammad Mehdi, Eghbalian Fatemeh, Emami Faranak, Abbasi Behnas, Zandevakili Hasan et al. Auditory Evaluation of High Risk Newborns by Automated Auditory Brain Stem Response. Iran J Pediatr. Dec 2008; 18 (4): 330-334.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


