Outcome of newborns born to mothers with prolonged rupture of membrane
Abstract
Introduction: Prolonged rupture of membrane (PROM) is an important risk factor for early onset neonatal sepsis (EONS), which is associated with increased neonatal morbidity and mortality. This study is mainly done to know the outcome of neonates born to mothers with history of PROM.
Methods: This study was conducted from January 2015 to December 2015 for a period of 12 months, in GSL medical college and hospital, Rajahmundry. Selection of cases-All the neonates born to mothers with history of prolonged rupture of membranes >18hrs were included in our study. Required investigations were done and followed during their hospital stay.
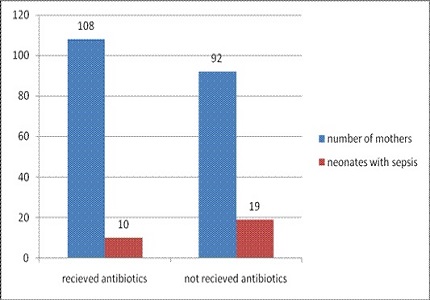
Results: Out of 200 neonates born to mothers with PROM, 60 had clinical sepsis, 29 had confirmed sepsis. Out of 29 confirmed cases of sepsis, positive blood culture was seen in 22 cases. The incidence of EONS in present study was found to be 14.5%. In present study neonatal sepsis had a higher rate of incidence in preterm neonates (61.5%) than in term neonates (38.5%). The incidence of neonatal sepsis was found to be lower in neonates born to mothers who took prenatal antibiotic treatment (9.25%) as compared to neonates born to mothers who did not receive prenatal antibiotic treatment (20.65%). Respiratory distress was the commonest presenting clinical sign (33 cases). Out of all the five Sepsis screen parameters C-Reactive Protein has the highest sensitivity (90.90%).
Conclusion: Preventive measures should focus on recognition of these high-risk infants with prompt laboratory screening for sepsis and early institution of empirical antibiotic based on local data
Downloads
References
2. World Health Report (2011): Level and trends in child mortality. Geneva: WHO 2011.
3. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Mathers C; Child Health Epidemiology Reference
Group of WHO and UNICEF. 2010 Jun 5;375(9730):1969-87. doi: 10.1016/S0140-6736(10)60549-1. Epub 2010 May 11.
4. Mahmood A, Fazal ur Rehman, Chughtai F. A survey of infection control practices in the delivery room and nursery to investigate and control the high rate of neonatal sepsis: an experience at a secondary care hospital. J Pak Med Assoc. 2008 May;58(5):237-40.
5. Popowski T, Goffinet F, Maillard F, Schmitz T, Leroy S, Kayem G. Maternal markers for detecting early-onset neonatal infection and chorioamnionitis in cases of premature rupture of membranes at or after 34 weeks of gestation: a two-center prospective study. BMC Pregnancy Childbirth. 2011 Apr 7;11:26. doi: 10.1186/1471-2393-11-26.
6. Kilbride HW, Thibeault DW. Neonatal complications of preterm premature rupture of membranes. Pathophysiology and management. Clin Perinatol. 2001 Dec;28(4):761-85.
7. Mercer BM, Goldenberg RL, Das AF, Thurnau GR, Bendon RW, Miodovnik M, Ramsey RD, Rabello YA; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. What we have learned regarding antibiotic therapy for the reduction of infant morbidity after preterm premature rupture of the membranes. Semin Perinatol. 2003 Jun;27(3):217-30. Review. [PubMed]
8. Medina TM, Hill DA. Preterm Premature Rupture of Membranes: Diagnosis and management. Am Fam Physician 2006;73:659-664. [PubMed]
9. Boskabadi H, Maamouri G, Mafinejad S (2011) Neonatal Complications Related with Prolonged Rupture of Membranes Macedonian Journal of Medical Sciences. 2011 Mar 15; 4(1):93-98. doi:10.3889/MJMS.1857-5773.2011.0159.
10. Mercer B. Antibiotics in the management of PROM and preterm labor. Obstet Gynecol Clin North Am. 2012 Mar;39(1):65-76. doi: 10.1016/j.ogc.2011.12.007. Epub 2012 Jan 28.
11. Al-Qa K, Al-Awaysheh F. Neonatal outcome and prenatal antibiotic treatment in premature rupture of membranes. Pak J Med Sci . 2005;21(4):441–444.
12. Assudani HJ, Gusani JK, Mehta SJ, Agravat HH, Kothari K. Bacteriological profiles of septicaemia in neonates at tertiary care hospital, Gujarat, India. J Res Med Den Sci.
(2015), [cited December 23, 2016]; 3(2): 148-151. doi:10.5455/jrmds.20153212.
13. Aletayeb SM, Khosravi AD, Dehdashtian M, Kompani F, Mortazavi SM, Aramesh RM. Identification of bacterial agents and antimicrobial susceptibility of neonatal sepsis: A 54-month study in a tertiary hospital. African Journal of Microbiology Research 2011;5(5): 528-31.
14. Cecilia CM, Mary AC, Elizabeth EG, Jonathan GL, Joanne JL et al. Etiology of neonatal sepsis in five urban hospitals in the Philippines. PIDSP Journal 2011;12(2):75-85.
15. Early Onset Neonatal Sepsis Betty Chacko and Inderpreet Sohi Neonatology Unit, Department of Pediatrics, Christian Medical College & Hospital, Ludhiana, Punjab, India. Indian J Pediatr 2005; 72 (1) : 23-26.
16. Yasmeen J. Al-Bayaa, Nedhal S.Ayoub , Sevan Najem Alwan. Relationship between Neonatal septicemia and birth weight. Fac Med Baghdad 2012;.54(2): 151-153.
17. Rajarshi Basu, Syamalkumar Bandyopadhyay. Study on Correlation between Sepsis Screening Blood Culture in Neonatal Sepsis. IOSR Journal of Dental and Medical Sciences May 2014;13( 5 ): 52-56. [PubMed]
18. Woranart Ratana Korn M.D., Witsanuchai Sri Jariya RPH. Ph.D (C) et al Incidence of neonatal infection in newborn infants with matneral history of premature rupture of membranes (PROM) for 18 houirs or longer .J Med Assoc. Thai 2005; 8 (7): 973-978. [PubMed]
19. Kifah Al-Qa Qa and Fatin Al-Awaysheh. Neonatal outcome and prenatal antibiotic treatment in premature rupture of membranes. Pak J Med Sci.2005; 21: 441-444.
20. Sanyal MK and Mukherjee TN. premature rupture of membrane; an assessment from a rural medical college of West Bengal; J. Obstet Gynecol India 1990; 40(4): 623-628.
21. Kodkany BS, Telang MA. Premature rupture of membranes. A study of 100 cases. J. Obstet Gynecol India 1991; 41(4): 492-496.
22. Sudan.Omer Saeed Magzoub , Mohamed Awadelkrim Ahmed , Yahia Shakir Abdelgadir. Clinical presentation of neonatal sepsis in paediatric ward at Khartoum North Teaching Hospital.Basic Research Journal of Medicine and Clinical Sciences. April 2015;4(4);116-120. [PubMed]
23. Jain NK, Jain VM, Maheshwari S. Clinical profile of neonatal sepsis. Kathmandu Univ Med J (KUMJ). 2003 Apr-Jun;1(2):117-20. [PubMed]
24. Setal B Chauhan, Viren Vaghasia, Bimal B Chauhan.C-Reactive Protein (CRP) in Early Diagnosis of Neonatal Septicemia..Natl J Med Res. 2012; 2(3): 276-278.
25. Boma A West,,Oliemen Peterside, Rosemary O Ugwu,and Augusta U Eneh. Prospective evaluation of the usefulness of C-reactive protein in the diagnosis of neonatal sepsis in a sub-Saharan African region. Antimicrob Resist Infect Control. 2012;1;22-26.
26. Neema Kayange, Erasmus Kamugish, Damas L Mwizamholya1, Seni Jeremiah and Stephen E Mshana. Kayange et al. Research article Predictors of positive blood culture and deaths among neonates with suspected neonatal sepsis in a tertiary hospital, Mwanza- Tanzania. BMC Pediatrics 2010; 10:39.
27. Eman M. Rabie Shehab El-Din, Mohamed M. Adel El-Sokkary, Mohamed Reda Bassiouny, and Ramdan Hassan.Epidemiology of Neonatal Sepsis and Implicated Pathogens: A Study from Egypt Hassan.BioMed Research International.2015;20:1-11.
28. A. S. Ahmed, M. A. Chowdhury, M. Hoque, and G. L. Darmstadt. Clinical and bacteriological profile of neonatal septicemia in a tertiary level pediatric hospital in Bangladesh. Indian Pediatrics 2002;39(11):1034–39.
29. J. Mugalu, M. K. Nakakeeto, S. Kiguli, and D. H. KadduMulindwa. Aetiology, risk factors and immediate outcome of bacteriologically confirmed neonatal septicaemia in Mulago hospital, Uganda. African Health Sciences.2006;6(2):120– 126. [PubMed]
30. F-Nilli and Shams Ansari A. Neonatal Complications of premature rupture of membrane. Acta Medica Iranica 2003;41(3) 176. [PubMed]
31. Ratanakorn W, Srijariya W, Chamnanvanakij S, Saengaroon P. Incidence of neonatal infection in newborn infants with a maternal history of premature rupture of membranes (PROM) for 18 hours or longer by using Phramongkutklao Hospital Clinical Practice Guideline (CPG). J Med Assoc Thai 2005 Jul;88(7):973-8. [PubMed]
32. Shashikala S. Tallur A. V. Kasturi, Shobha D. Nadgir, B. V. S. Krishna. Clinico-bacteriological study of neonatal septicemia in Hubli. Original Article. The Indian Journal of Pediatrics. 2000; 67(3); 169-174.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


