To study the efficacy of non-invasive ventilation in severe bronchiolitis
Abstract
Objectives: Bronchiolitis is the most common lower respiratory tract infection in infancy and about 6-15 % of patients of acute bronchiolitis require ventilatory support. Non Invasive Ventilation by increasing Mean Airway Pressure reduces airway resistance and recruits non-functional respiratory units to improve oxygenation. The objective of this study is to determine the effectiveness of Non Invasive Ventilation in patients of severe acute bronchiolitis.
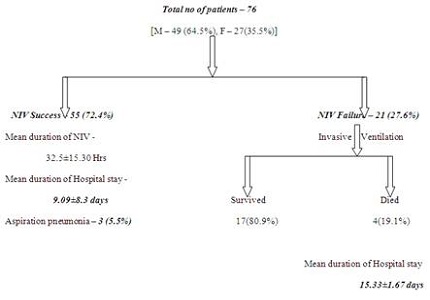
Methods: The present observational descriptive study was conducted in the department of Paediatrics, Dr. B.C. Roy Post Graduate Institute of Paediatric sciences, Kolkata, India. Those patients fulfilling the criteria for severe Acute Bronchiolitis according to Bronchiolitis Scoring System were included in this study. 76 patients were studied during the 1 year period from April 2014 to March 2015.
Results: A success rate of 72.4% has been observed in this study. Mean duration of Non Invasive Ventilation in patients where it was successful was 32.5±15.3 hours. Abnormalities in pH and PCO2 improved over a period of 6 hours.
Conclusion: Non Invasive Ventilation was found effective in 72.4% of patients of severe bronchiolitis. Abnormalities in pH & PCO2 were also improved over 6 hours. Thus, it is an effective, safe and cost effective modality of treatment of severe bronchiolitis.
Downloads
References
2. Paul VK, Bagga A, editors. Ghai Essential Pediatrics. 8th ed. NewDelhi:CBS Publishers & Distributors pvt Ltd;2013. Chapter 14, Disorders of Respiratory system; p.381-82.
3. Parthasarathy A, Menon PSN, Kundu R, editors. IAP Textbook of Pediatrics. 6th ed. NewDelhi:Jaypee Brothers Medical Publishers (p) Ltd;2013.Chapter 8.7, Bronchiolitis; p.565-68.
4. Martinón-Torres F. Current treatment for acute viral bronchiolitis in infants. Expert Opin Pharmacother. 2003 Aug;4(8):1355-71. [PubMed]
5. Kissoon N, Adderley R. Noninvasive ventilation in infants and children. Minerva Pediatr. 2008 Apr;60(2):211-8. [PubMed]
6. Gregoretti C, Pelosi P, Chidini G, Bignamini E, Calderini E. Non-invasive ventilation in pediatric intensive care. Minerva Pediatr. 2010 Oct;62(5):437-58. [PubMed]
7. Nizarali Z et al. Noninvasive ventilation in acute respiratory failure from respiratory syncytial virus bronchiolitis. Rev Bras TerIntensiva2012 Dec;24(4):375-380.
8. Teague WG. Noninvasive ventilation in the pediatric intensive care unit for children with acute respiratory failure. Pediatr Pulmonol. 2003 Jun;35(6):418-26.
9. Lazner MR, Basu AP, Klonin H. Non-invasive ventilation for severe bronchiolitis: analysis and evidence. Pediatr Pulmonol. 2012 Sep;47(9):909-16. doi: 10.1002/ppul.22513. Epub 2012 Feb 10. [PubMed]
10. Bronchiolitis – Clinical Practise Guidelines [Internet]. [cited 5 January 2017]. Available from: http://www.childrensdayton.org/cms/sitelet/e2f0864ef225ca51/index.html
11. Campion A et al. Non-invasive ventilation in infants with severe infection presumably due to respiratory syncytial virus: feasibility and failure criteria. Arch Pediatr. 2006 Nov;13(11):1404-9.
12. Nunes P, Abadesso C, Almeida E, Silvestre C, Loureiro H, Almeida H. [Non invasive ventilation in a pediatric intensive care unit]. Acta Med Port. 2010 May-Jun;23(3):399-404. Epub 2010 Jun 14. [PubMed]
13. Beasley JM, Jones SE. Continuous positive airway pressure in bronchiolitis. Br Med J (Clin Res Ed). 1981 Dec 5;283(6305):1506-8. [PubMed]
14. Essouri S et al. Improved clinical and economic outcomes in severe bronchiolitis with pre-emptive nCPAP ventilatory strategy. Intensive Care Med. 2014 Jan;40(1):84-91.
15. Milési C, Matecki S, Jaber S, Mura T, Jacquot A, Pidoux O, Chautemps N, Novais AR, Combes C, Picaud JC, Cambonie G. 6 cmH2O continuous positive airway pressure versus conventional oxygen therapy in severe viral bronchiolitis: a randomized trial. Pediatr Pulmonol. 2013 Jan;48(1):45-51. doi: 10.1002/ppul.22533. Epub 2012 Mar 19.
16. Essouri S et al. Optimal level of nasal continuous positive airway pressure in severe viral bronchiolitis. Intensive Care Med. 2011 Dec;37(12):2002-7.
17. Fleming PF, Richards S, Waterman K, Davis PG, Kamlin CO, Sokol J, Stewart M. Use of continuous positive airway pressure during stabilisation and retrieval of infants with suspected bronchiolitis. J Paediatr Child Health. 2012 Dec;48(12):1071-5. doi: 10.1111/j.1440-1754.2012.02468.x. Epub 2012 May 15.
18. Javouhey E, Barats A, Richard N, Stamm D, Floret D. Non-invasive ventilation as primary ventilatory support for infants with severe bronchiolitis. Intensive Care Med. 2008 Sep;34(9):1608-14. doi: 10.1007/s00134-008-1150-4. Epub 2008 May 24.
19. Thia LP, McKenzie SA, Blyth TP, Minasian CC, Kozlowska WJ, Carr SB. Randomised controlled trial of nasal continuous positive airways pressure (CPAP) in bronchiolitis. Arch Dis Child. 2008 Jan;93(1):45-7. Epub 2007 Mar 7.
20. Soong WJ,Hwang B,Tang RB. Continuous positive airway pressure by nasal prongs in bronchiolitis. Pediatr Pulmonol. 1993 Sep;16(3):163-6.
21. Oymar K, Bårdsen K. Continuous positive airway pressure for bronchiolitis in a general paediatric ward; a feasibility study. BMC Pediatr. 2014 May 12;14:122. doi: 10.1186/1471-2431-14-122. [PubMed]
22. Larrar S, Essouri S, Durand P, Chevret L, Haas V, Chabernaud JL, Leyronnas D, Devictor D. Effects of nasal continuous positive airway pressure ventilation in infants with severe acute bronchiolitis. Arch Pediatr. 2006 Nov;13(11):1397-403. Epub 2006 Sep 7.
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


