3 days vs. 7 days course of intravenous antibiotics for probable neonatal sepsis
Abstract
Introduction: Duration of appropriate antibiotic therapy for neonatal sepsis does not have evidence-based guidelines. The rationale and safety of these recommendations have never been scientifically evaluated. Such untested approaches could result in the unnecessary use of antibiotics leading to increased cost of care, unneeded intravenous cannulation, prolonged hospitalization, mother-infant separation, increased colonization by pathogenic organisms and emergence of drug resistant strains. So, our objective was to compare 3 days v/s. 7 days course of intravenous antibiotics for probable neonatal sepsis in order to determine the optimal length of antibiotic therapy so that infants with genuine infection would be adequately treated while those without infection would not be over-treated.
Methods: Randomized controlled trial (computerized randomization) done in the Neonatal Intensive Care Unit in a Tertiary care Teaching Hospital, Mysuru. About 150 neonates who were admitted in NICU for probable sepsis (clinical signs of sepsis and positive septic screening), who were on antibiotic therapy, with sterile blood culture at 3rd day of admission were the participants. Neonates who fulfilled the inclusion criteria were randomly divided into two groups, i.e; those who received 3 days of antibiotics and those who received 7 day course of antibiotics. Successful therapeutic outcome was measured in terms of weight gain, no apparent signs of sepsis as ascertained by clinical examination & no re hospitalization for sepsis.
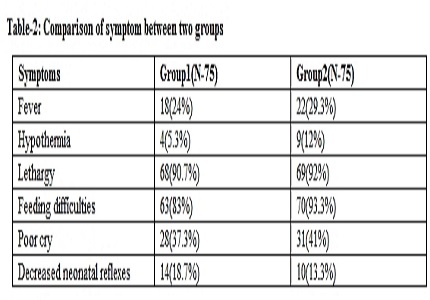
Results: Among the 150 eligible neonates in the study, (75 each in Groups 1 and 2, which were comparable with regard to term/preterm population and also early and late onset neonatal sepsis), there was no statistically significant difference in the outcome between the two groups in terms of mean age at presentation, gestational age, mode of delivery, age of onset of sepsis at presentation and relapse rates. However, the duration of hospital stay in group 1 babies who received 3 days of antibiotics was significantly shorter than in group 2 babies who received 7 days of antibiotics.
Conclusion: 3 day course of antibiotics is enough for culture sterile probable sepsis, in both term and preterm babies and also in both early and late onset neonatal sepsis.
Downloads
References
2. Klein JO. Bacterial sepsis and meningitis. In: Remington JS, Klein JO, editors. Infectious Diseases of Fetus and Newborn Infant. 5th Ed. Philadelphia: WB Saunders & Co. 2001.p.943-99.
3. Dear P. Neonatal infections: Infections in the newborn. In: Rinnie JM editor. Roberton’s Textbook of Neonatology. 4th ed. Elsevier Churchill Livingstone; 2005. p. 1011-1093.
4. Hammerschlag MR, Klein JO, Herschel M, Chen FC, Fermin R. Patterns of use of antibiotics in two newborn nurseries. N Engl J Med. 1977 Jun 2;296(22):1268-9. [PubMed]
5. Philip AG, Hewitt JR. Early diagnosis of neonatal sepsis. Pediatrics. 1980 May;65(5):1036-41. [PubMed]
6. Goldmann DA, Leclair J, Macone A. Bacterial colonization of neonates admitted to an intensive care environment. J Pediatr. 1978 Aug;93(2):288-93. [PubMed]
7. Lacey RW. Evolution of microorganisms and antibiotic resistance. Lancet. 1984 Nov 3;2(8410):1022-5. [PubMed]
8. Gordon A, Isaacs D. Late-onset infection and the role of antibiotic prescribing policies. Curr Opin Infect Dis. 2004 Jun;17(3):231-6.
9. Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Fishman NO. Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: risk factors for infection and impact of resistance on outcomes. Clin Infect Dis. 2001 Apr 15;32(8):1162-71. Epub 2001 Mar 26.
10. Gupta A. Hospital-acquired infections in the neonatal intensive care unit--Klebsiella pneumoniae. Semin Perinatol. 2002 Oct;26(5):340-5.
11. Royle J, Halasz S, Eagles G, Gilbert G, Dalton D, Jelfs P, et al. Outbreak of extended spectrum beta lactamase producing Klebsiella pneumoniae in a neonatal unit. Arch Dis Child Fetal Neonatal Ed. 1999; 80: F64-F68.
12. Pessoa-Silva CL, Meurer Moreira B, Camara Almeida V, Flannery B, Almeida Lins MC, Mello Sampaio JL, et al. Extended-spectrum beta-lactamase-producing Klebsiella pneumoniae in a neonatal intensive care unit: Risk factors for infection and colonization. J Hosp Infect. 2003; 53: 198-206.
13. Jain A, Roy I, Gupta MK, Kumar M, Agarwal SK. Prevalence of extended-spectrum beta-lactamase-producing Gram-negative bacteria in septicaemic neonates in a tertiary care hospital. J Med Microbiol. 2003 May;52(Pt 5):421-5.
14. Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sánchez PJ, Ambalavanan N, Benjamin DK Jr; NICHD Neonatal Research Network. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009 Jan;123(1):58-66. doi: 10.1542/peds.2007-3423.
15. Marra F, Lynd L, Coombes M, Richardson K, Legal M, Fitzgerald JM, Marra CA. Does antibiotic exposure during infancy lead to development of asthma?: a systematic review and metaanalysis. Chest. 2006 Mar;129(3):610-8. [PubMed]
16. Saini SS, Dutta S, Ray P, Narang A. Short course versus 7-day course of intravenous antibiotics for probable neonatal septicemia: a pilot, open-label, randomized controlled trial. Indian Pediatr. 2011 Jan;48(1):19-24. Epub 2010 Aug 1.
17. Kaiser JR, Cassat JE, Lewno MJ. Should antibiotics be discontinued at 48 hours for negative late-onset sepsis evaluations in the neonatal intensive care unit? J Perinatol. 2002 Sep;22(6):445-7. [PubMed]
18. Isaacs D, Wilkinson AR, Moxon ER. Duration of antibiotic courses for neonates. Arch Dis Child. 1987 Jul;62(7):727-8. [PubMed]
19. Ehl S, Gering B, Bartmann P, Högel J, Pohlandt F. C-reactive protein is a useful marker for guiding duration of antibiotic therapy in suspected neonatal bacterial infection. Pediatrics. 1997 Feb;99(2):216-21.
20. Bomela HN, Ballot DE, Cory BJ, Cooper PA. Use of C-reactive protein to guide duration of empiric antibiotic therapy in suspected early neonatal sepsis. Pediatr Infect Dis J. 2000 Jun;19(6):531-5.
21. Khashabi J, Karamiyar M, Taghinejhad H, Shirazi M. Use of Serial C-reactive Protein Measure-ments for Determination of the Length of Empiric Antibiotic Therapy in Suspected Neonatal Sepsis. Iranian Journal of Medical Sciences. 2015 Oct 4;29(1):31-5.
22. Lee WE, Chan ML, Young BWY. Reducing hospitalization and antibiotic use in suspected early neonatal sepsis through serial measurements of C-reactive proteins. HK J Pediatr. 2005;10:3-9.
23. Saxena S., Anand N.K., Saini L., et al. Bacterial infections among home delivered neonates. Clinical picture and bacteriological profile. Indian Pediatr. 1980 Jan;17(1):17-24.
24. Gupta P, Murali MV, Faridi MM, Kaul PB, Ramachandran VG, Talwar V. Clinical profile of klebsiella septicemia in neonates. Indian J Pediatr. 1993 Jul-Aug;60(4):565-72. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


