Growth and neurodevelopment outcome of NICUgraduates till 1 year at a tertiary care centre in eastern India and identification of the clinical and electrophysiological predictors of adverse developmental outcome
Abstract
Background: Despite serious neonatal morbidity, the neurodevelopmental outcome of NICU (Neonatal Intensive Care Unit) graduates is often reasonably good. Infants with neurodevelopmental abnormality need to start therapy early, and hence, they should be detected as soon as possible. Therefore we need well designed follow-up services.
Objectives: To study the outcome of growth and development till one year of age of NICU graduates from a tertiary care centre in eastern India.
Design and setting: A prospective neurodevelopmental follow-up study on graduates from the Calcutta National Medical College and Hospital NICU.
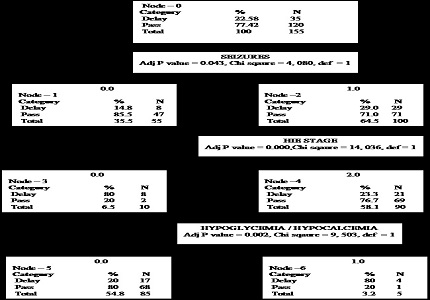
Methodology: We selected a cohort of 177 consecutive NICU graduates according to high-risk criteria and followed them up at the high risk clinic of Paediatrics department up to 1 year of age on a predetermined schedule. Growth monitoring (weight, length, head circumference measurements), neurologic examination by Amiel-Tison method, developmental assessment using Denver Development Screening Test (DDST) as screening tool and Developmental Assessment Scale for Indian Infants (DASII) as a definitive test, neuroimaging (cranial ultrasound or magnetic resonance imaging of brain) and electrophysiological investigations visual evoked potential (VEP), brainstem auditory evoked response (BAER), and electroencephalogram (EEG) were done. Early stimulation and physiotherapy were advised as per need. Ongoing illnesses were identified and treated.
Results: Out of 177 consecutive NICU graduates enrolled in the study, 155 were followed up to 1 year of age. There were no statistically significant difference in the occurrence of growth failure, and neurodevelopmental delay between term and preterm and between appropriate for gestational age (AGA) and small for gestational age (SGA) infants. However growth failure was significantly higher among infants with neurodevelopmental delay.
Conclusion: Persistence of abnormalities in tone, BAER, EEG & neuroimaging strongly predicted adverse neurodevelopmental outcome. Recurrent respiratory tract infection was found to be the most common morbidity among NICU graduates followed by seizure disorder.
Downloads
References
2. Milner KM, Neal EFG, Roberts G, Steer AG, Duke T. Long-term neurodevelopmental outcome in high-risk newborns in resource-limited settings: a systematic review of the literature. Paediatrics and International Child Health 2015;35:227-242.
3. Nair MK, Philip E, Jeyaseelan L, George B, Mathews S, Padma K. Effect of Child Development Centre model early stimulation among at risk babies--a randomized controlled trial. Indian Pediatr. 2009 Jan;46 Suppl:s20-6.
4. Chaudhari S, Kulkarni S, Barve S, Pandit AN, Sonak U, Sarpotdar N. Neurologic sequelae in high risk infants--a three year follow up. Indian Pediatr. 1996 Aug;33(8):645-53. [PubMed]
5. Paul VK, Radhika S, Deorari AK, Singh M. Neurodevelopmental outcome of 'at risk' nursery graduates. Indian J Pediatr. 1998 Nov-Dec;65(6):857-62. [PubMed]
6. Sukumaran TU, Vijesh PV, Sukumaran PS. Developmental delay and disabilities in high risk newborns- a follow up study. Journal of Rehabilitation Council of India 2008 Jan-Dec;4(1&2):18-24.
7. Baburaj S, Abraham B, Vasant PV, Raj S et al. Growth and development till one year from a rural neonatal intensive care unit in south India. Int J Biomed Reseach 2013;4(12):695-700.
8. Luo YF, Zheng K, Zhou XJ, Liang JF. Mental development of high-risk neonates:a long-term follow-up study. World J Pediatr 2006 May 15;2:121-124.
9. Molteno CD, Thompson MC, Buccimazza SS, Magasiner V, Hann FM. Evaluation of the infant at risk for neurodevelopmental disability. S Afr Med J. 1999 Oct;89(10):1084-7. [PubMed]
10. Galbraith RS, Derrick EJ. The value of entry criteria in follow-up clinics for neonatal intensive care unit graduates. Paediatr Child Health 1998;3:169–172.
11. Chaudhari S, Bhalerao M, Chitale A, Patil B, Pandit A, Hoge M. Transient tone abnormalities in high risk infants and cognitive outcome at five years. Indian Pediatr. 2010 Nov;47(11):931-5. Epub 2010 Jan 15. [PubMed]
12. Perat M, Russman BS, Budden S. Cerebral Palsy and its co-morbidity- Follow up of High Risk Neonates. Paper presented at: The Asia Pacific Childhood Disability Update; 2005 Dec 2-4; Mumbai, India. P. 59-66.
13. Campos M, Reyes G, García L. Comparison of postdischarge growth in adequate for gestational age and small for gestational age very low birthweight infants. Ethn Dis. 2008 Spring;18(2 Suppl 2):S2-118-22. [PubMed]
14. Newman DG, O'Callaghan MJ, Harvey JM, Tudehope DI et al. Characteristics at four months follow-up of infants born small for gestational age: a controlled study. Early Hum Dev.1997;49:169-181. [PubMed]
15. Yau KI, Chang MH. Growth and body composition of preterm, small-for-gestational-age infants at a postmenstrual age of 37-40 weeks. Early Hum Dev. 1993 Jun;33(2):117-31. [PubMed]
16. Godbole K, Barve S, Chaudhari S. Early predictors of neurodevelopmental outcome in high risk infants. Indian Pediatr. 1997 Jun;34(6):491-5. [PubMed]
17. Begum HA, Rahman A, Anowar S, Mortuza A, Nahar N. Long term outcome of birth asphyxiated infants. Mymensingh Med J. 2006 Jan;15(1):61-5. [PubMed]
18. Padayachee N, Ballot DE. Outcomes of neonates with perinatal asphyxia at a tertiary academic hospital in Johannesburg, South Africa. South African Journal of Child Health 2013 Mar 26;7:89-94.
19. Mukhopadhyay K, Chowdhary G, Singh P, Kumar P, Narang A. Neurodevelopmental outcome of acute bilirubin encephalopathy. J Trop Pediatr. 2010 Oct;56(5):333-6. doi: 10.1093/tropej/fmp142. Epub 2010 Feb 1.
20. Bhakoo ON, Kumar P, Sheikh S. Prematurity in India. What does the future hold? J Neonatol 2007; 21:79-81.
21. Chaudhari S, Kulkarni S, Pajnigar F, Pandit AN, Deshmukh S. A longitudinal follow up of development of preterm infants. Indian Pediatr. 1991 Aug;28(8):873-80. [PubMed]
22. Modi M, Saluja S, Kler N, Batra A, Kaur A, Garg P, Soni A, Suman P. Growth and neurodevelopmental outcome of VLBW infants at 1 year corrected age. Indian Pediatr. 2013 Jun 8;50(6):573-7. Epub 2012 Nov 5.
23. Berry ALA, Bellig LL. Neonatal sepsis- follow up. J Pediatr 2008;153:160-163.
24. Beligere N, Rao R. Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. J Perinatol. 2008 Dec;28 Suppl 3:S93-101. doi: 10.1038/jp.2008.154.
25. Procianoy RS, Koch MS, Silveira RC. Neurodevelopmental outcome of appropriate and small for gestational age very low birth weight infants. J Child Neurol. 2009 Jul;24(7):788-94. doi: 10.1177/0883073808331087. Epub 2009 Mar 16.
26. Mukhopadhyay K, Malhi P, Mahajan R, Narang A. Neurodevelopmental and behavioral outcome of very low birth weight babies at corrected age of 2 years. Indian J Pediatr. 2010 Sep;77(9):963-7. doi: 10.1007/s12098-010-0149-3. Epub 2010 Sep 3. [PubMed]
27. Sanders R, Durieux-Smith A, Hyde M, Jacobson J, Kileny P, Murnane O. Incidence of hearing loss in high risk and intensive care nursery infants. J Otolaryngol Suppl. 1985 Feb;14:28-33. [PubMed]
28. Maqbool M, Najar BA, Gattoo I, Chowdhary J. Screening for Hearing Impairment in High Risk Neonates: A Hospital Based Study. J Clin Diagn Res. 2015 Jun;9(6):SC18-21. doi: 10.7860/JCDR/2015/14509.6104. Epub 2015 Jun 1. [PubMed]
29. Fakharee SH, Kazemian M, Hamedieh AA. Hearing assessment of the high risk neonate admitted to Mofid Hospital for children during 2001-2002, using ABR. Arch Iranian Med 2004;7:44-46.
30. Misra PK, Katiyar CP, Kapoor RK, Shukla R, Malik GK, Thakur S. Brainstem auditory evoked response in neonates with birth asphyxia. Indian Pediatr. 1997 Mar;34(3):199-205. [PubMed]
31. Sharma P, Chhangani NP, Meena KR, Jora R, Sharma N, Gupta BD. Brainstem evoked response audiometry (BAER) in neonates with hyperbilirubinemia. Indian J Pediatr. 2006 May;73(5):413-6. [PubMed]
32. Agrawal VK, Shukla R, Misra PK, Kapoor RK, Malik GK. Brainstem auditory evoked response in newborns with hyperbilirubinemia. Indian Pediatr. 1998 Jun;35(6):513-8. [PubMed]
33. Shah S, Fernandez AR, Chirla D. Role of brain spect in neonates with hypoxic ischemic encephalopathy and its correlation with neurodevelopmental outcome. Indian Pediatrics 2001;38(7):705-713.
34. Sauve R, Aziz K, Davis D, Lee SK, Ohlsson A. Routine screening cranial ultrasound examinations for the prediction of long term neurodevelopmental outcomes in preterm infants. Paediatr Child Health. 2001;6:39–43.
35. Amess P, McFerran C, Khan Y, Rabe H. Early prediction of neurological outcome by term neurological examination and cranial ultrasound in very preterm infants. Acta Paediatr. 2009 Mar;98(3):448-53.
36. Zeinstra E, Fock JM, Begeer JH, van Weerden TW, Maurits NM, Zweens MJ. The prognostic value of serial EEG recordings following acute neonatal asphyxia in full-term infants. Eur J Paediatr Neurol. 2001;5(4):155-60.
37. Hussain N, Clive J, Bhandari V. Current incidence of retinopathy of prematurity, 1989-1997. Pediatrics. 1999 Sep;104(3):e26. [PubMed]
38. Doyle LW, Anderson PJ, Battin M, Bowen JR, Brown N, Callanan C, Campbell C, Chandler S, Cheong J, Darlow B, Davis PG, DePaoli T, French N, McPhee A, Morris S, O'Callaghan M, Rieger I, Roberts G, Spittle AJ, Wolke D, Woodward LJ. Long term follow up of high risk children: who, why and how? BMC Pediatr. 2014 Nov 17;14:279. doi: 10.1186/1471-2431-14-279. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


