Outcome analysis of intussusception in fifty children at a tertiary centre in Mumbai
Abstract
Background: Intussusception is a common cause of obstruction in Paediatric patients. Recognizing and treating this condition rapidly is important to prevent potentially fatal complications.
Methods: Fifty consecutive patients of intussusception were analyzed with respect to age, presenting symptoms with duration, laboratory and radiological findings, type of management, duration of hospital stay and follow-up.
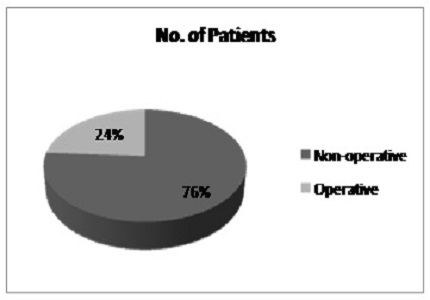
Results: The median age at presentation was 11 months. Patients presenting between 3 months and 2 years of age are more likely to require operative intervention. The most common presenting symptoms were abdominal pain and vomiting. The diagnosis of intussusception was made by Ultrasonography and a trial of non-operative intervention was given first by in the form of USG guided hydrostatic reduction. Most of the patients required two or lesser attempts of reduction and were thus managed non-operatively. Those who did not respond to 2 or more attempts of hydrostatic reduction required operative intervention and all of these had some or the other lead point. Eight out of 11 operated patients (72.72%) required resection for the gangrenous bowel segment. The most common type of intussusception was ileo-colic and most of them were idiopathic. Lead points were found in all the patients who were operated; the most common being enlarged mesenteric lymph nodes.
Conclusion: Children presenting between 3 months to 2 years of age, with no palpable abdominal lump or passage of red currant jelly-like stools as symptoms and getting reduced hydrostatically at one or two attempts mostly have idiopathic intussusception and such patients won’t require operative intervention.
Downloads
References
2. Paul M. Columbani and Stephen Scolz: Paediatric Surgery seventh edition. P. 1093-1110. [PubMed]
3. Young DG. Intussusception. in: O'Neil JA Jr, Rowe MI, Grosfeld JL, Fonkalsrud EW, Coran AG, editors. Pediatric Surgery. 5th ed. Mosby, New York, USA. 1998. p. 1185-98.
4. Dennison WM. Acute intussusception in infancy and childhood. Glasgow Med J. 1948 Mar;29(3):71-80. [PubMed]
5. Jen H C,Shew S B : the impact of hospital type and experience on the operative utilization in paediatric intussusception: A nationwide study. J Pediatric Surg 2009; 44: 241-6. [PubMed]
6. Daneman A, Navarro O. Intussusception. Part 2: an update on the evolution of management. Pediatr Radiol 2004;34:97-108. [PubMed]
7. Katz M, Phelan E, Carlin JB, et al. Gas enema for the reduction of intussusception: relationship between clinical signs and symptoms and outcome. AJR Am J Roentgenol 1993;160:363-6. [PubMed]
8. Bratton S L, Haberkern C M, Waldhausen J H et al. Intussusception : Hospital size and risk of surgery. Paediatrics 2001; 107: 299-303. [PubMed]
9. Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol 2009;15:407-11. [PubMed]
10. Saxena AK, Hollwarth ME. Factors influencing management and comparison of outcomes in paediatric intussusceptions. Acta Paediatr 2007;96:1199-202. [PubMed]
11. Fraser JD, Aguayo P, Ho B, et al. Laparoscopic management of intussusception in pediatric patients. J Laparoendosc Advanced Surg Techn 2009;19:563-5. [PubMed]
12. Kaiser AD, Applegate KE, Ladd AP. Current success in the treatment of intussusception in children. Surgery 2007;142:469-75. [PubMed]
13. Kodikara H, Lynch A, Morreau P, et al. Ten-year review of intussusception at Starship Hospital: 1998–2007. N Z Med J 2010;123:32-40. [PubMed]
Copyright (c) 2015 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


