Clinico-etiological profile and outcome of traumatic head injury in children- a tertiary care experience
Abstract
Introduction: Children are most vulnerable to head injury, which is one of the most common indications for hospitalization and is often associated with significant morbidity and mortality in severe cases. This study was undertaken to know about the clinical profile, etiology and outcome of head injury in children in a tertiary care hospital.
Study Design: Retrospective study.
Materials and method: This study was done on 53 children with head injury admitted to pediatric department of Velammal Medical College, Madurai from October 2013- December 2016.
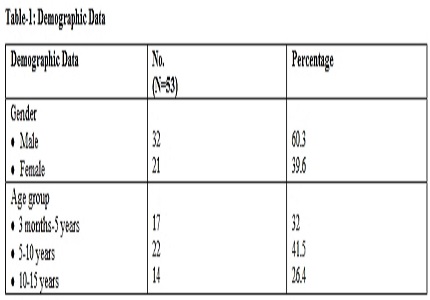
Results: Out of the 53 children studied with head injury, males outnumbered (60.3%) females (39.6%). Road traffic accident was the most common cause of head injury (52.8%), followed by accidental fall (47.1%). Vomiting was the most common symptom at admission (58.4%) followed by injuries to scalp and face (41.5%) headache (37.7%), altered sensorium (28.3%). Head injury was mild in severity in 71.6% of childer. Neuro-imaging analysis showed traumatic brain injury in (73.5%) of them, skull bone fractures in (49%), facial bone fractures in (15%) of children. Outcome was measured as with full recovery in 86.7% of children, (5.6%) had partial recovery, death in 3.7% of children.
Conclusion: Parental guidance is advised to avoid accidental falls. Implementation of strict traffic rules, timely intervention and aggressive management reduces morbidity and mortality in children with traumatic head injury.
Downloads
References
2. Ghizoni E, Ade FM, Baracat EC, Joaquim AF, Fraga GP, Rizoli S, etal. Indications for head computed tomography in children with mild traumatic brain injury. Rev Col Bras Cir 2013;Nov-Dec;40(6):515-9. [PubMed]
3 Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Atabaki SM, Holubkov R, etal. Identification of children at very low risk of clinically important brain injuries after head trauma: a prospective cohort study. Lancet. 2009 Oct 3;374(9696):1160-70. doi: 10.1016/S0140-6736(09)61558-0. Epub 2009 Sep 14.
4. Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002 Jan;16(1):15-27.
5. Max JE, Friedman K, Wilde EA, Bigler ED, Hanten G, Schachar RJ, etal. Psychiatric disorders in children and adolescents 24 months after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci 2015;27 (2) :112-120. https://doi:10.1176/appi.neuropsych.13080190.
6. Jurado EA, Paulsen JS, Ehly S, Max JE. Traumatic Brain Injury in Children and Adolescents: Academic and Intellectual Outcomes Following Injury. Exceptionality 2006;14(3): 125-140.
7. Maw A, Tasker R, Bateman A, Gracey F, Kieta F, Bower R, etal. Mild and moderate traumatic brain injury in childhood – who gets admitted?. Pediatric neurology ACNR 2011;11( 5):14-16.
8. Harwood-Nash DC, Hendrick EB, Hudson AR. The significance of skull fractures in children. Radiology 1971;Oct 101(1):151-156. http://pubs.rsna.org/doi/pdf/10.1148/101.1.151
9. Arneitz C, Sinzig M, Fasching G. Diagnostic and Clinical Management of Skull Fractures in Children. J Clin Imaging Sci. 2016;6:47. [PubMed]
10. Kapapa T, Kapapa M, Posovszky C, Gulke J, Konig R, Woischneck D, Wirtz CR, Pala A. Paediatric Head Injury: The Incidence of Multiple Injuries. Journal of Behavioral and Brain Science. 2016 Jun;6(6):254-267. https://dx.doi.org/10.4236/jbbs.2016.66026.
11. Kumar M, Hussain M, Saeed S, Huda MF, Usmani JA. Head injuries sustained by children due to fall from height: A comprehensive study. J Indian Acad Forensic Med.Oct-Dec 2013; 35 (4 ) :305-307.
12. Erhasin Y, Mutluer S, Mirzai H, Palali I. Pediatric depressed skull fractures: analysis of 530 cases. Childs Nerv Syst 1996 Jun; 12( 6): 323-31.
13. Morris KP, Forsyth RJ, Parslow RC, Taskar RC, Hawley CA. Intracranial pressure complicating severe traumatic brain injury in children:monitoring and management. Intensive care med 2006 Oct;32(10):1606-12. https://doi:10.1007/s00134-006-0285-4.
14. Park SH, Cho B, Oh SM. Head injuries from falls in preschool children. Yonsei Med J 2004;45 (2): 229-232. [PubMed]
15. Ibrahim NG, Wood J, Margulies SS, Christian CW. Influence of age and fall type on head injuries in infants and toddlers. Int. J. Devl. Neurosci 2012 May ;30(3):201-6. doi:10.1016/j.ijdevneu.2011.10.007. [PubMed]
16. Tascu A, Pascal C, Lencean M, Gorgan MR. Aggressive or conservative management in extradural hematomas in children-a challenging neurosurgical choice. Romanian Neurosurgery 2014;4: 384-393. https://doi.org/10.2478/romneu-2014-0054
17. Cole P, Kaufman Y, Hollier LH. Managing the pediatric facial fracture. Craniomaxillofac Trauma Reconstr. 2009 May;2(2):77-83. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


