Clinical and hematological profile of sickle cell disease affected children in rural tertiary level hospital
Abstract
Introduction: Sickle cell disease is commonly seen in rural population of western part of India. It is one of the common causes of recurrent hospitalization, morbidity and mortality in pediatric population. As there are limited studies addressing the pattern of sickle cell disease amongst pediatric population, this study was taken up to evaluate the clinicohematological profile of pediatric population with sickle cell disease in a rural tertiary care hospital in western part of India.
Methods: This was a retrospective observational study. Data was retrieved from pediatric sickle cell clinic of the department. Data of children diagnosed with sickle cell disease from June 2013 to September 2016 was collected and analyzed to assess the hematological profile at the time of diagnosis and to find if there was any correlation between various hemoglobin variants and the hematological parameters.
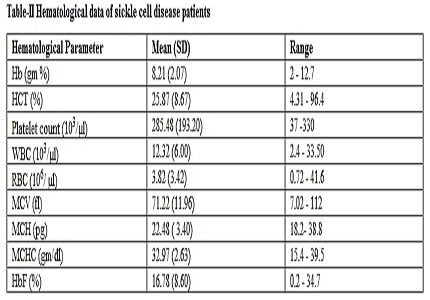
Results: About 173 patients were included in the study. Vasoocclusive crisis was the most common presentation (43.93 %) followed by generalized body ache joint pain (36.99 %) and acute febrile illness (26.39 %), while 45 (26.01%) patients presented with severe anemia. Hematological finding was suggestive of moderate anemia, low Mean corpuscular volume and low Mean hemoglobin concentration.
Conclusion: At the time of diagnosis vasoocclusive crisis and generalized bodyache are the most common manifestations in pediatric population with sickle cell disease while hematological picture is suggestive of microcytic hypochromic anemia. There is a positive correlation between age at presentation and severity of anemia at the time of diagnosis.
Downloads
References
2. Stevens MC, Hayes RJ, Vaidya S, Serjeant GR . Fetal hemoglobin and clinical severity of homozygous sickle cell disease in early childhood. J Pediatr. 1981 Jan;98(1):37-41.
3. Lehmann H, Cutbush M. Sickle cell trait in southern India. Br Med J.1952 Feb 23; 1(4755):404–5. [PubMed]
4. Negi RS (1972) Sickle cell trait in India. A review of known distribution. Bull Anthropol Survey India.1972;17:439–49.
5. Maier-Redelsperger M, de Montalembert M, Flahault A, et al. Fetal hemoglobin and F-cell responses to long-term hydroxyurea treatment in young sickle cell patients. The French Study Group on Sickle Cell Disease. Blood. 1998;91(12):4472-9.
6. M. Kamble and P. Chatruvedi. Epidemiology of Sickle cell diseae in a rural hospital of central India .Indian Pediatrics 2000;37(4): 391- 6.
7. Chukwu BF, Ezenwosu OU, Eke CB, Chinawa JM, Ikefuna AN, et al. What Factors Influence the Age at Diagnosis of Sickle Cell Anemia in Enugu, Nigeria? J Blood Disord Transfus. 2014; 5:231.doi: 10.4172/2155-9864.1000231.
8. Sumanta Panigrahi P. K. Patra, P. K. Khodiar. The Screening and Morbidity Pattern of Sickle Cell Anemia in Chhattisgarh Indian J Hematol Blood Transfus. 2015 Mar; 31(1):104–9. doi: 10.1007/s12288-014-0407-z.
9. Subramaniam S, Chao JH.Managing Acute Complications of Sickle Cell Disease In Pediatric Patients.Pediatr Emerg Med Pract. 2016 Nov;13(11):1-28. [PubMed]
10. Kar BC, Satapathy RK, Kulozik AE, Kulozik M, Sergeant BE. Sickle Cell disease in Orissa State, India. Lancet 1986; 2: 1198-1201. [PubMed]
11. Mandot S, Khurana LV, Sonesh JK (2009) Sickle cell anemia in Garasia Tribals of Rajasthan. Indian Pediatrcs 2009 Mar; 46(3):239-40. [PubMed]
12. Sahu T, Sahani NC, Das S et al (2003) Sickle cell anemia in tribal children of Gajapati district in southern Orissa. Indian J Commun Med; 28:180–183.
13. Balgir RS (2005) Spectrum of hemoglobinopathies in state of Orissa, India: a ten years Cohort Study. JAPI 2005; 53:1021–26. [PubMed]
14. Samal GC. Sickle cell crisis: Hematological changes. Indian Pediatr 195; 22: 121-124. [PubMed]
15. Goswmai Sankar, Das Kishore K.. Socio-economic and demographic determinants of childhood anemia. J. Pediatr. (Rio J.) 2015 Oct ;29 : 91( 5 ): 471-7. [PubMed]
16. Roy B, Dey B, Balgir RS, et al. Identification of sickle cell homozygotes using haematological parameters. J Indian Anthrop Soc. 1996;31:191–9.
17. Tshilolo L, Wembonyama S, Summa V, Avvisati G. Hemogram findings in Congolese children with sickle cell disease in remission] Med Trop (Mars) 2010;70:459–63. [PubMed]
18. Rao SS, Goyal JP, Raghunath SV, Shah VB. Hematological profile of sickle cell disease from South Gujarat, India. Hematology Reports. 2012;4(2):e8. doi:10.4081/hr.2012.e8. [PubMed]
19. Kaur M, Das GP, Verma IC. Sickle cell trait and disease among tribal communities in Orissa, Madhya Pradesh and Kerala. Indian J Med Res. 1997;55:104–9. [PubMed]
20. Mohanty D, Mukherjee MB, Colah RB, et al. Iron deficiency anaemia in sickle cell disorders in India. Indian J Med Res. 2008 Apr;127:366–9. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


