Environmental risk factors for childhood asthma in a Semi-urban area of Western Tamilnadu
Abstract
Introduction: Environmental determinants are integral part of etiology, severity and management of asthma. But the association between various indoor and outdoor triggers with pediatric asthma has been inconsistent, complex and variable across the globe. This study was aimed at identifying the environmental risk factors associated with childhood asthma in our region.
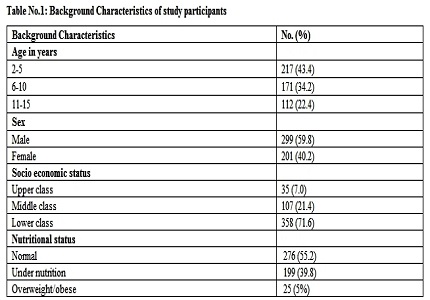
Methods: This was a hospital-based cross-sectional study done at Perundurai Medical college hospital, Tamilnadu. After getting Institutional Ethical Committee approval, children in the age group of 2 to 15 years attending the pediatric outpatient department were enrolled in the study. Parents were interviewed with ISAAC questionnaire and history of exposure to various indoor and outdoor triggers was recorded in addition to the basic demographic details and anthropometric indices. Data was analyzed using Chi-square tests and logistic regression analysis.
Results: Among 500 subjects, 298 (59.6%) were asthmatics and 202 (40.4%) were non-asthmatics. Age group of 6-10 years (OR 1.94, 95% CI 1.20- 3.13), male gender (OR 2.26, 95% CI 1.47-3.48), overweight/obesity (OR 3.70, 95% CI 1.17-11.66), mould (OR 2.43, 95% CI 1.37- 4.32), seasonal variation (OR 2.39, 95% CI 1.51-3.79) and outdoor air pollution (OR 6.17, 95% CI 4.00- 9.53) were independently associated with childhood asthma. Passive smoking, type of cooking fuel, absence of smoke outlet, exposure to animals and proximity of house to arterial road were not significantly associated with asthma.
Conclusion: Environmental triggers play a significant role in pediatric asthma. Appropriate interventions to mitigate these modifiable risk factors would decrease the burden of the disease substantially.
Downloads
References
2. Reddel HK, Bateman ED, Becker A, Boulet LP, Cruz AA, Drazen JM, Haahtela T, Hurd SS, Inoue H, de Jongste JC, Lemanske RF Jr, Levy ML, O'Byrne PM, Paggiaro P, Pedersen SE, Pizzichini E, Soto-Quiroz M, Szefler SJ, Wong GW, FitzGerald JM. A summary of the new GINA strategy: a roadmap to asthma control. Eur Respir J. 2015 Sep;46(3):622-39. doi: 10.1183/13993003.00853-2015. Epub 2015 Jul 23.
3. Marks G, Pearce N, Strachan D, Asher I. Global burden of disease due to asthma. In: The Global Asthma Report 2014. Auckland, New Zealand: Global Asthma Network, 2014. p. 16-21.
4. Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006 Nov 23;355(21):2226-35. [PubMed]
5. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, Williams H; ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006 Aug 26;368(9537):733-43. [PubMed]
6. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet. 1998 Apr 25;351(9111):1225-32.
7. Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ. 2009 Oct 27;181(9):E181-90. doi: 10.1503/cmaj.080612. Epub 2009 Sep 14. [PubMed]
8. Wang HY, Wong GW, Chen YZ, Ferguson AC, Greene JM, Ma Y, Zhong NS, Lai CK, Sears MR. Prevalence of asthma among Chinese adolescents living in Canada and in China. CMAJ. 2008 Nov 18;179(11):1133-42. doi: 10.1503/cmaj.071797.
9. Liu AH, Covar RA, Spahn JD, Sicherer SH. Childhood asthma. In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, editors. Nelson textbook of pediatrics. New Delhi (India): Reed Elsevier India; 2016. p.1097.
10. Strachan DP. The role of environmental factors in asthma. Br Med Bull. 2000;56(4):865-82. [PubMed]
11. Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, et al. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology 2012 Aug;17(6):887-98. doi:10.1111/j.1440-1843.2012.02195.x.
12. Chakravarthy S, Singh RB, Swaminathan S, Venkatesan P. Prevalence of asthma in urban and rural children in Tamil Nadu. Natl Med J India. 2002 Sep-Oct;15(5):260-3. [PubMed]
13. Dhabadi BB, Athavale A, Meundi A, Rekha R, Suruliraman M, Shreeranga A, Gururaj S. Prevalence of asthma and associated factors among schoolchildren in rural South India. Int J Tuberc Lung Dis. 2012 Jan;16(1):120-5. doi: 10.5588/ijtld.11.0195.
14. Kumar SG, Premarajan KC, Sarkar S, Sahu SK, Sahana, Ambika, et al. Prevalence and factors associated with asthma among school children in rural Puducherry, India. Curr Pediatr Res 2012;16(2):159–63.
15. Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995 Mar;8(3):483-91. [PubMed]
16. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: World Health Organization, 2006 (312 pages).
17. Khadilkar VV, Khadilkar AV. Revised Indian Academy of Pediatrics 2015 growth charts for height, weight and body mass index for 5-18-year-old Indian children. Indian J Endocrinol Metab. 2015 Jul-Aug;19(4):470-6. doi: 10.4103/2230-8210.159028.
18. Oberoi SS. Updating income ranges for Kuppuswamy's socio-economic status scale for the year 2014. Indian J Public Health. 2015 Apr-Jun;59(2):156-7. doi: 10.4103/0019-557X.157540. [PubMed]
19. Johnson CC, Ownby DR, Zoratti EM, Alford SH, Williams LK, Joseph CL. Environmental epidemiology of pediatric asthma and allergy. Epidemiol Rev. 2002;24(2):154-75.
20. Apelberg BJ, Aoki Y, Jaakkola JJ. Systematic review: Exposure to pets and risk of asthma and asthma-like symptoms. J Allergy Clin Immunol. 2001 Mar;107(3):455-60. [PubMed]
21. Jain A, Vinod Bhat H, Acharya D. Prevalence of bronchial asthma in rural Indian children: a cross sectional study from South India. Indian J Pediatr. 2010 Jan;77(1):31-5. doi: 10.1007/s12098-009-0308-6. Epub 2010 Jan 20.
22. George CE, Chopra H, Garg SK, Bano T, Jain S, Kumar A. Environmental correlates of bronchial asthma in children in a slum of Meerut – A cross-sectional study. Int J Med Res Rev 2014 Sep-Oct;2(5):469-473. doi:10.17511/ijmrr.2014.i05.012.
23. Kozyrskyj AL, Kendall GE, Jacoby P, Sly PD, Zubrick SR. Association between socioeconomic status and the development of asthma: analyses of income trajectories. Am J Public Health. 2010 Mar;100(3):540-6. doi: 10.2105/AJPH.2008.150771. Epub 2009 Aug 20.
24. Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007 Apr 1;175(7):661-6. Epub 2007 Jan 18. [PubMed]
25. Pekkanen J, Hyvärinen A, Haverinen-Shaughnessy U, Korppi M, Putus T, Nevalainen A. Moisture damage and childhood asthma: a population-based incident case-control study. Eur Respir J. 2007 Mar;29(3):509-15. Epub 2006 Nov 15. [PubMed]
26. Won YK, Hwang TH, Roh EJ, Chung EH. Seasonal patterns of asthma in children and adolescents presenting at emergency departments in Korea. Allergy Asthma Immunol Res 2016 May;8(3):223-9. doi:10.4168/aair.2016.8.3.223.
27. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014 May 3;383(9928):1581-92. doi: 10.1016/S0140-6736(14)60617-6. [PubMed]
28. McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, Künzli N, Gauderman J, Avol E, Thomas D, Peters J. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006 May;114(5):766-72. [PubMed]
29. Strachan DP, Cook DG. Health effects of passive smoking. 6. Parental smoking and childhood asthma: longitudinal and case-control studies. Thorax. 1998 Mar;53(3):204-12. [PubMed]
30. Kumar GS, Roy G, Subitha L, Sahu SK. Prevalence of bronchial asthma and its associated factors among school children in urban Puducherry, India. J Nat Sci Biol Med. 2014 Jan;5(1):59-62. doi: 10.4103/0976-9668.127289.
31. Singh D, Sobti PC, Arora V, Soni RK. Epidemiological study of asthma in rural children. Indian J Community Med 2002 Oct-Dec;27(4):167-70.
32. Zheng T, Niu S, Lu B, Fan X, Sun F, Wang J, Zhang Y, Zhang B, Owens P, Hao L, Li Y, Leaderer B. Childhood asthma in Beijing, China: a population-based case-control study. Am J Epidemiol. 2002 Nov 15;156(10):977-83. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


