Study of Osteomyelitis in paediatric patients
Abstract
Introduction: Osteomyelitis is defined as inflammation of bone. Though the main culprits are bacteria occasionally fungi may also be involved. Prognosis of untreated or delayed treatment onset osteomyelitis is often bad and leads to adverse outcomes. Very few cases of osteomyelitis are reported from India as compared to other infectious conditions. In this study we aim to study the number of patients, male: female ratio, type of osteomyelitis and the bacterial profile associated with osteomyelitis.
Methods: After obtaining Institutional Ethics approval, the present study was conducted from 1st January 2016 - 31st December 2016 at KVG Medical College, Sullia. Blood and sample like fluid aspirate or discharge collected was subjected to microscopy and culture. Antibiotic susceptibility testing was done using disk diffusion methods. Radiological data of the patients was also collected.
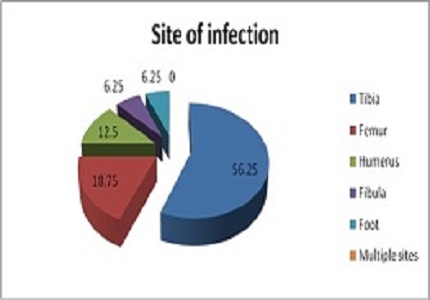
Results: Bacteria were isolated from 32 cases. The most affected age group was of 6-10 years of age (46.87%). Males were more affected as compared to females and male: female ratio was 3:1. Maximum number of patients were of acute osteomyelitis (87.5%) followed by subacute osteomyelitis (9.38%) and chronic osteomyelitis was found in just a single patient (3.12%). Long bones like tibia (56.25%), femur (18.75%), humerus (12.5%) were mostly affected. Blood culture was positive in 65.62% cases. Methicillin Sensitive Staphylococcus Aureus (MSSA) was the most common isolate (56.25%) followed by, Methicillin Resistant Staphylococcus Aureus (MRSA), Acinetobacter, Coagulase Negative Staphylococcus(CONS), Streptococcus pyogens, E.coli and Pseudomonas.
Conclusion: Thus, S. aureus was the most common cause of acute bacterial osteomyelitis and mostly affected school age group children.
Downloads
References
2. Lew DP, Waldvogel FA. Osteomyelitis. N Engl J Med. 1997 Apr 3;336(14):999-1007. [PubMed]
3. Jansson A, Jansson V, von Liebe A. [Pediatric osteomyelitis]. Orthopade. 2009 Mar;38(3):283-94. doi: 10.1007/s00132-008-1402-6. [PubMed]
4. Ronald M. Laner and Carol B. Lindsley. Infectious arthritis and osteomyelitis. Section 5, Chapter 37-Arthritis related to infection. Available from: http://peds.stanford.edu/Rotations/red_team/pdfs/JIA/Cassidy-Petty%20Infectious%20Arthritis%20and%20Osteomyelitis.pdf
5. Diana Gomes, Margarida Pereira, Ana Francisca Bettencourt. Osteomyelitis: an overview of antimicrobial therapy. Brazilian Journal of Pharmaceutical Sciences. 2013; 49(1):13-27. Doi: 10.1590/S1984-82502013000100003.
6. Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004 Jul 24-30;364(9431):369-79. [PubMed]
7. Gutierrez K. Bone and joint infections in children. Pediatr Clin North Am. 2005 Jun;52(3):779-94, vi. [PubMed]
8. Dich VQ, Nelson JD, Haltalin KC. Osteomyelitis in infants and children. A review of 163 cases. Am J Dis Child. 1975 Nov;129(11):1273-8. [PubMed]
9.Darville T, Jacobs RF. Management of acute hematogenous osteomyelitis in children. Pediatr Infect Dis J. 2004 Mar;23(3):255-7. [PubMed]
10. Pedro Fiorini Puccini, Maria Aparecida G. Ferrarini, Antônio Vladir Iazzetti. Pediatric acute hematogenous osteomyelitis: analysis of patients assisted in a university hospital. Rev Paul Pediatr. 2012;30(3):353-8. DOI: 10.1590/S0103-05822012000300008.
11. Peltola H, Pääkkönen M. Acute osteomyelitis in children. N Engl J Med. 2014 Jan 23;370(4):352-60. doi: 10.1056/NEJMra1213956. [PubMed]
12. Harik NS, Smeltzer MS. Management of acute hematogenous osteomyelitis in children. Expert Rev Anti Infect Ther. 2010 Feb;8(2):175-81. doi: 10.1586/eri.09.130. [PubMed]
13. Hatzenbuehler J, Pulling TJ. Diagnosis and management of osteomyelitis. Am Fam Physician. 2011 Nov 1;84(9):1027-33. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


