A study on neonatal apnea in relation to etiopathogenesis and their outcome in a rural based Medical College Hospital;West Bengal; India
Abstract
Introduction: Neonatal apnea is one of the most common causes of Sick Newborn Care Unit and Neonatal Intensive Care Unit admission. Commonest etiologies of neonatal apnea include sepsis, apnea of prematurity, central nervous system insult, Respiratory distress Syndrome.
Background: Apnea in neonates may be manifestation of many serious underlying diseases as well as may be due to prematurity. Apnea of prematurity is essentially a diagnosis of exclusion carries the most excellent prognosis. Other secondary causes bear uniformly poor prognosis and essentially high mortality.
Objectives: This study was conducted in a tertiary care centre to determine the different causes of apnea and to observe the outcome in relation to different birth weight, gestational age and different etiologies.
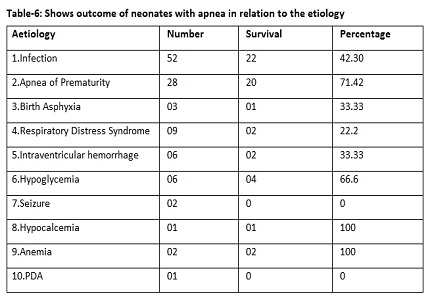
Results: Out of 110 apneic neonates recruited 60% had ≥ 3 episodes of apnea while 40% had 1-2 episodes. Sepsis and apnea of prematurity were found to be the two most common causes. Average birth weight and gestational age for the sepsis group was 1598•62 gm and 32•4 wks respectively whereas average birth weight and gestational age for apnea of prematurity group was 1094•07 gm and 30•0 wks respectively. Survival rate for babies with apnea of prematurity (71•42%) was better than babies with infection (42•3%).
Conclusion: All babies born below 32 weeks of gestational age must undergo close monitoring for apnea. Neonates with apneic spells should be evaluated to exclude secondary causes of apnea like sepsis, hypoglycaemia and intracranial hemorrhage etc., because sepsis remains the commonest cause of apnea and carries a poor prognosis.
Downloads
References
2. Ann R stark, John P Cloherty , Erice Eichenwald Apnea, Manual of Neonatal Care, 7th edition 2011.
3. Rigatto H, Maturation of breathing. Clinical perinatology. 1992; 19(4):739-56. [PubMed]
4. Haddad G. Respiratory control in the newborn: comparative physiology and clinical disorders. In: Mathew OP, Respiratory control and disorders in the newborn. New York: Marcel Dekker,2003:1-13. [PubMed]
5. Ruggins NR. Pathophysiology of apnoea in preterm infants. Arch Dis Child. 1991 Jan;66(1 Spec No):70-3. [PubMed]
6. Reid DH, Tunstall ME. Recurrent Neonatal Apnoea. Lancet. 1965 Jul 24;2(7404):155-6.
7. Gabriel M, Albani M. Cardiac slowing and respiratory arrest in preterm infants. Eur J Pediatr. 1976 Jul 12;122(4):257-61.
8. Hiatt IM, Hegyi T, Indyk L, Dangman BC, James LS. Continuous monitoring of PO2 during apnea of prematurity. J Pediatr. 1981 Feb;98(2):288-91.
9. Poet CF, Stebbens VA, Samuels MP, Southall DP: The relationship between bradycardia, apnea, and hypoxemia in preterm infants. Pediatr Res 34:144,1993. [PubMed]
10. Miriam E Tucker, OB/GYN News: June 2003.
11. Pediatric Pulmonology, 2008, volume 43, Issue 10, pages 937-944, Jalal M. Abu- Shaweesh MD, Richard J. Martin MD. [PubMed]
12. The late preterm infant and the control of breathing, sleep, and brainstem development: A review; Clin Perinatol. 2006;33(4): 883-914; abstract x (ISSN: 0095-5108) Darnall RA; Arigno RL; Kinney HC.
13. Gozal D, New concepts in abnormalities of respiratory control on children. Current Opinion in Pediatrics. 2004; 16(3):305-8.
14. Upton CJ, Milner AD, Stokes GM. Apnoea, bradycardia, and oxygen saturation in preterm infants. Arch Dis Child. 1991 Apr;66(4 Spec No):381-5.
15. Joshi A, Gerhardt T, Shandloff P, Bancalari E. Blood transfusion effect on the respiratory pattern of preterm infants. Pediatrics. 1987 Jul;80(1):79-84.
16. Westkamp E; Soditt V; Adrian S; Bohnhorst B; Groneck P; Pets CF, Department of Neonatology, Kinderkrankenhaus Amsterdame Strasse, Köln,Germany Blood transfusion in anemic infants with apnea of prematurity. Biology of Neonates. 2002;82(4):228-32.
17. Kattwinkel J, Mars H, Fanaroff AA, Klaus MH. Urinary biogenic amines in idiopathic apnea of prematurity. J Pediatr. 1976 Jun;88(6):1003-6.
18. Kurlak LO, Ruggins NR, Stephenson TJ. Effect of nursing position on incidence, type, and duration of clinically significant apnoea in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1994 Jul;71(1):F16-9.
19. Rajiv Aggarwal, Ashwini Singhal, Ashok K Deorari and Vinod K. Paul, Apnea in the Newborn, Indian Jornal of Pediatrics,vol-68-Oct2001. [PubMed]
20. Scanlon JE, Chin KC, Morgan ME, Durbin GM, Hale KA, Brown SS. Caffeine or theophylline for neonatal apnoea? Arch Dis Child. 1992 Apr;67(4 Spec No):425-8.
21. Steer PA, Henderson-Smart DJ(2002). Caffeine versus theophylline for apnea in preterm infants Cochrane Database of Systemic Reviews.
22. Waldemer A: Apnea, Respiratory tract disorders, Nelson Textbook of Pediatrics,19thedition,2012,p580-81.
23. Speidel BD, Dunn PM. Use of nasal continuous positive airway pressure to treat severe recurrent apnoea in very preterm infants. Lancet. 1976 Sep 25;2(7987):658-60.
24. Jones RA, Lukeman D. Apnoea of immaturity. 2. Mortality and handicap. Arch Dis Child. 1982 Oct;57(10):766-8. [PubMed]
25. Pillekamp F, Hermann C, Keller T, von Gontard A. Kribs A, Roth B. Factors influencing apnea and bradycardia of prematurity, Neonatology 2007;91:155-161.
26. Pilcher G, Urlesberger B, Muller W(2003) Impact of bradycardia on cerebral oxygenation and cerebral blood volume during apnoea in preterm infants. Physiol Meas 24(3):671-680.
27. Janvier A, Khairy M, Kokkotis A, Cormier C, Messmer D, Barrington KJ. J Perinatol. 2004 Dec;24(12):763-8. [PubMed]
28. Narang A, Gathwala G, Kumar P. Apnea in neonates. Indian Pediatr. 1997 Apr;34(4):329-31. [PubMed]
29. Naeye RL. Neonatal apnea: underlying disorders. Pediatrics. 1979 Jan;63(1):8-12. [PubMed]
30. Klein J Nizet V. Bacterial sepsis and meningitis: Infectious Disease of the Fetus and Newborn infant.7thed.2011,p244.
31. Fanaroff AA et al; Incidence, presenting features, risk factors and significance of late onset Septicemia in very low birth weight infants.Pediatr infect Dis 17: 593,1998. [PubMed]
32. Thomas N. Hansen and Anthony Corbet, Control of Breathing, Avery disease of the Newborn, 9th edition 2011.
33. Henderson- Smart DJ; Butcher- Puech MC; Edwards DA, Incidence and mechanism of bradycardia during apnoea in preterm infants. Archives of Disease in Childhood. BMJ,1986;61(3):227-32.
34. Barbara J. Stoll and Robert M. Kliegman, Respiratory tract disorders, Apnea,Nelson Textbook of Pediatrics 17thed.2004. 573-574.
35. Henry L Halliday, Pulmonary disorder and apnea, Forfar and Arneil’s text book of pediatrics 2003.
36. Kenneth M Hunter, Metabolic Bone Disease of prematurity: John P Cloherty, Eric C Eichenwald, Ann. R. Stark, Manual of Neonatal Care,7th ed.2011.
37. Gerhardt T, Bancalari E. Apnea of prematurity: I. Lung function and regulation of breathing. Pediatrics. 1984 Jul;74(1):58-62. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


