Magnitude, clinical spectrum and etiology of hepatobiliary disorders in children- a tertiary care experience
Abstract
Objectives: This study was undertaken to know about the magnitude, clinical spectrum and etiology of liver diseases in children in a tertiary care teaching hospital.
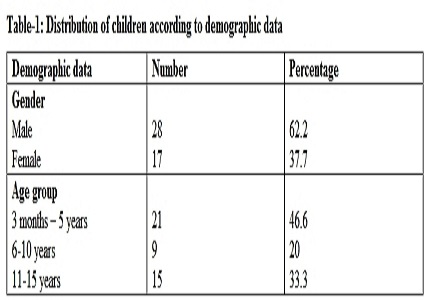
Materials and Methods: This is a hospital based, retrospective, descriptive study. It was done on 45 children with hepatobiliary diseases admitted to pediatric department of Velammal Medical College, Madurai from Jan 2016 – Dec 2016.
Results: As about 45 children out of 2259 pediatric admissions, had hepatobiliary disorders. This was contributing to 1.99% of total admissions. Liver function test was deranged in (73.3%) of children. Males (62.2%), outnumbered, females (37.7%) in our study. Children less than 5 years of age were most commonly affected (46.6%). Most common symptom in children with hepatobiliary disorders were jaundice (51.1%), nausea/vomiting (46.6%), anorexia (40%), pain abdomen (33.3%), high coloured urine (28.8%), bleeding manifestations and abdomen distension in (20%) each, fever in (17.7%), failure to thrive and irritability in (15.5%) each. The most common sign observed was icterus (51.1%), hepatomegaly (42.2%). Ascitis and splenomegaly was noted in (26.6%) each, edema in (20%) and pallor in (15.5%) of children. Acute liver diseases were more common (68.8%) than chronic liver diseases (31.1%). The most common etiology of acute liver disease was acute viral hepatitis (28.8%), cholelithiasis (22.2%), non-alcoholic fatty liver disease (6.6%), liver abscess (4.4%), acute viral hepatitis with acalculous cholecystitis in (4.4%), acute liver failure due to paracetamol poisoning in (2.2%) of children. Etiology noted for chronic liver diseases were biliary atresia (13.3%), idiopathic cirrhosis and wilsons disease in (6.6%) each, autoimmune hepatitis and chronic hepatitis in (2.2%) each.
Conclusion: Since age is the single most important determinant in successful management of biliary atresia, recognition and definitive identification of the condition as the cause of neonatal cholestasis syndrome in a given case very early after the onset of symptoms is of paramount importance.
Downloads
References
2. Ahamed PA, Ulonnam CC, Mohammed-Nafiu R, Ballong J, Nwankwo G. Pattern of liver diseases among children attending the National Hospital Abuja, Nigeria. Niger J Paed 2016;43(1):46-50.
3. Dar GA, Zarger SA, Jan K, Malik MI, Mir TA, Dar MA. Spectrum of Liver diseases among children in kashmir valley. Academic medical journal of India. 2014 Nov 20;2(3):80-86.
4. Wieckowska A, Feldstein AE. Nonalcoholic fatty liver disease in the pediatric population: a review. Curr Opin Pediatr. 2005 Oct;17(5):636-41. [PubMed]
5. Tahir A, Malik FA, Ahmad I, Krishin J, Akhtar P. Aetiological factors of chronic liver disease in children. J Ayub Med Coll Abbottabad 2011;23(2):12-14. https://www.ayubmed.edu.pk/JAMC/23-2/Awais.pdf
6. Hanif M, Raza J, Qureshi H, Issani Z. Etiology of chronic liver disease in children. J Pak Med Assoc. 2004 Mar;54(3):119-22. [PubMed]
7. Pinto RB, Schneider AC, da Silveira TR. Cirrhosis in children and adolescents: An overview. World J Hepatol. 2015 Mar 27;7(3):392-405. doi: 10.4254/wjh.v7.i3.392. [PubMed]
8. Nayak NC, Vasdev N. Neonatal cholestasis syndrome: identifying the disease from liver biopsy. Indian Pediatr. 2002 May;39(5):421-5.
9. Karim MB, Rahman MM, Islam MS. Wilsons disease with hepatic presentation in childhood. Mymensingh Med J. 2007 Jan;16(1):29-32. [PubMed]
10. Yuce A, Kocak N, Gurakan F, Ozen H. Wilsons disease with hepatic presentation in childhood. Indian Pediatr. 2000 Jan;37:31-36. [PubMed]
11. Sabir OM. Pathologic causes of liver disease in Sudanese children: Results of 450 liver needle biopsies at a single children hospital. Sudan J Paediatr. 2011;11(1):38-41. [PubMed]
12. Dhole SD, Kher AS, Ghildiyal RG, Tambse MP. Chronic Liver Diseases in Children: Clinical profile and Histology. Journal of Clinical and Diagnostic Research. JCDR. 2015;9(7):SC04-SC07.
13. Monajemzadeh M, Tabriz HM, Mahjoub F, Fallahi G, Farahmand F. Liver needle biopsy in Iranian pediatric patients: diagnostic significance and pattern of liver diseases. Indian J Pathol Microbiol. 2009 Jan-Mar;52(1):10-3.
14. Dangwal TR, Aggarwal V, Malhotra V, Baveja U, Mittal SK. Clinical spectrum of chronic liver disease in north Indian children. Trop Gastroenterol. 1997 Oct-Dec;18(4):174-6. [PubMed]
15. Williams R. Classification, etiology, and considerations of outcome in acute liver failure. Semin Liver Dis. 1996 Nov;16(4):343-8. [PubMed]
16. Ramakrishna B, Date A, Kirubakaran C, Raghupathy P. The pattern of liver disease in Indian children: a review of 128 biopsied cases. Ann Trop Paediatr. 1993;13(2):159-63. [PubMed]
17. Muthuphei MN. Childhood liver diseases in Ga-Rankuwa Hospital, South Africa. East Afr Med J. 2000 Sep;77(9):508-9. [PubMed]
18. Akinbami FO, Venugopalan, Nirmala V, Suresh J, Abiodun P. Pattern of chronic liver disease in Omani children- a clinicopathological review. West Afr J Med.2004 Apr-Jun;23(2):162-6.
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


