Study on clinico-serological profile of juvenile idiopathic arthritis in children
Abstract
Background: Chronic arthritis, the most common chronic rheumatic disease of childhood, is one of the more frequent chronic illnesses of children. Besides clinical examination, various hematological and immunological markers are being used to diagnose Juvenile Idiopathic Arthritis (JIA). The present study was designed to be conducted in our institution to find out the clinico-serological profile of JIA.
Materials and Methods: All children under 14 years, attending the OPD and suspected to be suffering from Juvenile Idiopathic Arthritis, during September 2010 to September 2012 were included in the study. They were screened for the diagnosis of JIA. All the cases were subjected to hematological, immunological, biochemical and radiological investigation. Analysis was made on clinico-serological profile of the disease.
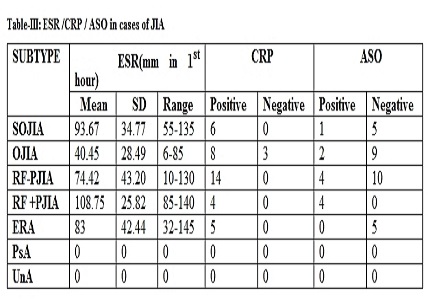
Results: Majority out of 40 cases belonged to the age group 5-10 years and males out-numbered the females. Pallor was present in 100% of SOJIA and Polyarticular RF +ve JIA, 78.5% in Polyarticular RF –ve JIA, and 60% of Enthesitis related arthritis (ERA). In systemic onset JIA, soft tissue swelling was found in 66.67% cases. No cases of psoriatic arthritis or undifferentiated types were detected. Juxta articular osteoporosis was found in 66.67% cases. Methotrexate, Oral steroid and Hydroxychloroquine were the drugs used for most of the varieties of JIA.
Conclusion: Even though, different varieties of JIA were detected, no cases of psoriatic arthritis or undifferentiated types were found. Chronic arthritis in childhood shows very diverse clinical pattern. JIA is like an iceberg, the diagnosis of which is usually missed due to lack of definite diagnostic parameters and less accessibility of the common man to the health facility.
Downloads
References
2. David M. Siegel, MPH; Harry L. Gewanter, Juvenile idiopathic arthritis, American Academy of Pediatrics Textbook of Pediatric Care, 2009.
3. Eveline Y. Wu, Heather A. Van Mater, C. Egla Rabinovich, Juvenile Idiopathic Arthritis, Nelson Textbook of Pediatrics,19th ed,2011:329-339.
4. Demirkaya E, Ozen S, Bilginer Y, Ayaz NA, Makay BB, Unsal E, et al. The distribution of juvenile idiopathic arthritis in the eastern Mediterranean: results from the registry of the Turkish Paediatric Rheumatology Association. ClinExpRheumatol 2011; 29: 111–6.
5. Stabile A, Avallone L, Compagnone A, Ansuini V, Bertoni B, Rigante D. Focus on juvenile idiopathic arthritis according to the 2001 Edmonton revised classification from the International League of Associations for Rheumatology: an Italian experience. Eur Rev Med Pharmacol Sci. 2006 Sep-Oct;10(5):229-34. [PubMed]
6. Kunjir V, Venugopalan A, Chopra A. Profile of Indian patients with juvenile onset chronic inflammatory joint disease using the ILAR classification criteria for JIA: a community-based cohort study. J Rheumatol. 2010 Aug 1;37(8):1756-62. doi: 10.3899/jrheum.090937. Epub 2010 Jun 1.
7. Seth V, Kabra SK, Semwal OP, Jain Y. Clinico-immunological profile in juvenile rheumatoid arthritis--an Indian experience. Indian J Pediatr. 1996 May-Jun;63(3):293-300. [PubMed]
8. Aggrawal A, Mishra R. Juvenile chronic arthritis in India: Is it different from that seen in Western countries ? Rheum Int 1994; 14 ; 53‐56.
9. Alsufyani K, Ortiz‐Alvarez O, Cabral DA, et al. The role of subcutaneous administration of methotrexate in children with juvenile idiopathic arthritis who have failed oral methotrexate. J Rheumatol 2004; 31(1): 179–82. [PubMed]
10. Hunt PG, Rose CD, McIlvain-Simpson G, Tejani S. The effects of daily intake of folic acid on the efficacy of methotrexate therapy in children with juvenile rheumatoid arthritis. A controlled study. J Rheumatol. 1997 Nov;24(11):2230-2. [PubMed]
11. Burgos‐Vargas R, Vazquez‐Mellado J, Pacheco‐Tena C, et al. A 26 week randomised, double blind, placebo controlled exploratory study of sulfasalazine in juvenile onset spondyloarthropathies. Ann Rheum Dis 2002; 61: 941–2.
12. Ilowite NT. Current treatment of juvenile rheumatoid arthritis. Pediatrics. 2002 Jan;109(1):109-15. [PubMed]
13. Broström E, Hagelberg S, Haglund-Akerlind Y. Effect of joint injections in children with juvenile idiopathic arthritis: evaluation by 3D-gait analysis. Acta Paediatr. 2004 Jul;93(7):906-10.
14. Ruperto N, Murray KJ, Gerloni V, et al. Pediatric Rheumatology International Trials Organization. A randomized trial of parenteral methotrexate comparing an intermediate dose with a higher dose in children with juvenile idiopathic arthritis who failed to respond to standard doses of methotrexate. Arthritis Rheum. 2004 Jul;50(7):2191-201. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


