Clinical profile and outcome of children with severe acute malnutrition
Abstract
Introduction: Severe Acute Malnutrition (SAM) is a unique type of severe malnutrition and is different from severe underweight and severe stunting. This study evaluated the clinical manifestations among the children admitted to the SCB medical college and SVP PGIP and elucidated further the factors associated with severe malnutrition among the undernourished children and finally the outcome in terms of cured or mortality.
Materials and Methods: This hospital-based cross-sectional time-bound study with follow-up component was conducted by using technique of sampling without replacement. Children aged 1-60 months admitted to SCB MCH and SVPPGIP during September 2013 to September 2015, having features of SAM were considered for the study population. After detailed history and physical examination, relevant investigations were done and critical analysis made.
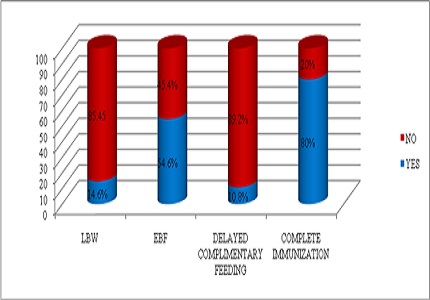
Results: Total 130 patients with SAM constituted the study population. The overall prevalence of SAM was 2.5 %. Majority were non edematous SAM (Marasmus) (77%) and rest were oedematous (Kwashiorkor).There was no variation in sex as both male and female patients were with equal percentage (50%). About 12.3 % of children with SAM were less than 2 months, 47.7 % between 2 to 12 months, and 40% were above 12 months.
Conclusion: Malnutrition is predicted by age less than two years, living with single parent, taking unbalanced diet, lack or incomplete immunization and low level of maternal education. Co-morbidities associated with malnutrition were pneumonia, pulmonary tuberculosis, urinary tract infection. Mortality is predicted by age less than one year, peasant parents, having severe malnutrition, dehydration, hypothermia, and hypoglycemia.
Downloads
References
2. de Onís M, Monteiro C, Akré J, Glugston G. The worldwide magnitude of protein-energy malnutrition: an overview from the WHO Global Database on Child Growth. Bull World Health Organ. 1993;71(6):703-12. [PubMed]
3. Amsalu S, Tigabu Z. Risk factors for severe acute malnutrition in children under the age of five: A case-control study. Ethiop.J.Health Dev.2008; 22:21-25.
4. World Health Organization, Country Office For India; National Rural Health Mission(IN). Facility Based Care of Severe Acute Malnutrition: Participant Manual.(New Dehli): World Health Organization, Country Office for India; 2011 Mar. 119p.
5. Irena AH, Mwambazi M, Mulenga V. Diarrhea is a Major killer of Children with Severe Acute Malnutrition admitted to inpatient set-up in Lusaka. Nutrition Journal.2011; 10:110.
6. Ministry of Health and Family Welfare, Government of India (2011) Operational Guidelines on Facility-Based Management of Children with Severe Acute Malnutrition.New Delhi: National Rural Health Mission, Ministry of Health and Family Welfare.
7. Aguayo VM, Jacob S, Badgaiyan N, Chandra P, Kumar A, Singh K. Providing care for children with severe acute malnutrition in India: new evidence from Jharkhand. Public Health Nutrition. 2012; 1-6.
8. Owor M, Tumwine JK, Kikafunda JK. Socio-economic risk factors for severe protein energy malnutrition among children in Mulago Hospital, Kampala. East Afr Med J. 2000 Sep;77(9):471-5. [PubMed]
9. Roy SK, Buis M, Weersma R, Khatun W, Chowdhury S, Begum A, Sarker D, Thakur SK, Khanam M. Risk factors of mortality in severely-malnourished children hospitalized with diarrhoea. J Health Popul Nutr. 2011 Jun;29(3):229-35. [PubMed]
10. Mahgoub HM, Adam I. Morbidity and mortality of severe malnutrition among Sudanese children in New Halfa Hospital, Eastern Sudan. Trans R Soc Trop Med Hyg. 2012 Jan;106(1):66-8. doi: 10.1016/j.trstmh.2011.09.003. Epub 2011 Oct 22.
11. Mahgoub SEO, Nnyepi M, Bandeke T. Factors Affecting Prevalence of Malnutrittion among Children under Three Years of Age in Botswana.Afr J Food AgrNutr Dev. 2006;6(1):1–15.
12. Kleynhans, I.C., MacIntyre, U.E. and Albertse, E.C. 2006. Stunting among young black children and the socio-economic and health status of their mothers/caregivers in poor areas of rural Limpopo and urban Gauteng – the NutriGro Study. South African Journal of Clinical Nutrition. Vol. 19. no. 4. pp.163-172.
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


