A study of Co- morbidities in children aged 6 months to 12 years receiving multiple blood transfusions
Abstract
Background: Transfusion of blood and blood products is an established way of treating patients who are deficient in one or more blood component.
Aim &objective: Blood transfusion is a vital therapeutic measure which influences the outcome of transfusion dependent subjects. Although survival has increased in these subjects parallel to advances in chemotherapy and chelating, they are more prone to acquiring various co morbidities like transfusion transmitted infection (TTI), transfusion associated adverse event, and iron overload leading to a negative impact on quality and duration of life of the patients.
Objective: To assess the consequences of multiple blood transfusions, leading to incidence of co morbidities in recipients.
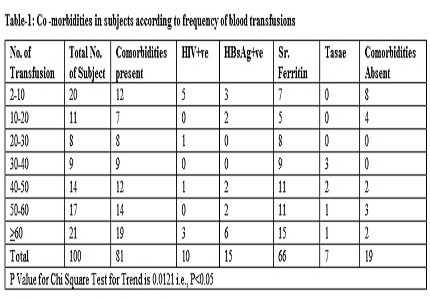
Method: the present study entitled co morbidities in patients receiving multiple transfusions is a descriptive Study and has been carried out in institute during the period of February 2015 to February 2016. Patients receiving multiple blood transfusions were categorized as hemolytic disease and non-hemolytic disease. Patients were screened for transfusion transmitted infection like HIV and HBs Ag, serum ferrites.
Result: out of 100 subjects, 86 had hemolytic disease and 14 had non hemolytic disease. The study performed showed that out of 98 total co- morbidities, increased serum ferritin contributed to 67.35%, HIV to 10.20%, HbsAg to 15.31% and 7.14% was contributed by Transfusion Associated Serious Adverse Events (TASAE).
Conclusion: Blood transfusion can lead to severe adverse effects which can cause temporary or permanent morbidity.
Downloads
References
2. Jain V,Lokesh Mr. Sachdera A. Prevention of Thalessemia.In Hemoglobinopathies. Sachdeva A,Lokeshwar Mr.Shaha N,Agarwal BR,Khama VK,Yadav SP, et al editors.New Delhi : Japee brothers medical publishers(pvt)Ltd:2006 P.95.
3. Giri, P.A,Deshpande,J.D,Phalke,D.B and Karle,L.B(2012)Seroprevalance of transfusion transmissible infections among voluntary blood donors at a territory care teaching hospital in rural area of India Journal of family medicine and primary care,1-48-51.
4. Slonim AD, Joseph JG, Turenne WM, Sharangpani A, Luban NL. Blood transfusions in children: a multi-institutional analysis of practices and complications. Transfusion. 2008 Jan;48(1):73-80. Epub 2007 Sep 24. [PubMed]
5. Blundell J.Observation on transfusion of blood by Dr Blundell with a description of his graviator.Lancet 1828,(ii):321-4.
6. Amar Apuker DN,Kumar A.Vaidya Murti P,Bichile SK,Kairo RH,et al,Frequency of hepatitis B,C and D and human immune deficiency virus infections in multi transfused thalessemia Indian J Gastroenterology 1992;11:80-1.
7. Lukuni ML,Binda P,Mbensa 1,Seroprevalance of HIV infected children with sickle cell anemia.Infant AIDS 1994 Aug 7-12;10:253.
8. Ocak S, Kaya H, Cetin M, Gali E, Ozturk M. Seroprevalence of hepatitis B and hepatitis C in patients with thalassemia and sickle cell anemia in a long-term follow-up. Arch Med Res. 2006 Oct;37(7):895-8. [PubMed]
9. Vinelli E, Lorenzana I. Transfusion-transmitted infections inmulti-transfused patients in Honduras. J Clin Virol. 2005 Dec;34 Suppl 2:S53-60.
10. Karimi M, Ghavanini AA. Seroprevalence of hepatitis B, hepatitis C and human immunodeficiency virus antibodies among multitransfused thalassaemic children in Shiraz, Iran. J Paediatr Child Health. 2001 Dec;37(6):564-6.
11. Lee WS,The CM, Chan LL. Risk of sereconversion of hepatits B,hepatitis C and human immune efficiency viruses in children with multi transfused thalessemia major J paediatric child health 2005;41:265-8.
12. Pomper GJ. Febrile,allergic and nonimmune transfusion reactions.In: Rossi’s principles of transfusion medicine.4th ed.Simon TL,Synder EL,Solheim BG,Stowell CP,Strauss RG,Petrides M,editors.Oxford,UK:Willy-Blackwell Publishing Ltd.;2009.p.826-46.
13 .Ward JW, Bush TJ, Perkins HA, Lieb LE, Allen JR, Goldfinger D, Samson SM, Pepkowitz SH, Fernando LP, Holland PV, et al. The natural history of transfusion-associated infection with human immunodeficiency virus. Factors influencing the rate of progression to disease. N Engl J Med. 1989 Oct 5;321(14):947-52.
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


